Hyperglycemia
Published .
Clinically, hyperglycemia is blood glucose greater than 125 mg/dL while fasting and greater than 180 mg/dL 2 hours after eating. A patient has impaired glucose tolerance, or pre-diabetes, with a fasting plasma glucose of 100 mg/dL to 125 mg/dL.
When hyperglycemia is left untreated, it can lead to many serious life-threatening complications that include damage to the eye, kidneys, nerves, heart, and peripheral vascular system. Thus, it is vital to manage hyperglycemia effectively and efficiently to prevent complications of the disease and improve patient outcomes.
Etiology
Factors contributing to hyperglycemia include reduced insulin secretion, decreased glucose utilization, and increased glucose production. Glucose homeostasis is a balance between hepatic glucose production and peripheral glucose uptake and utilization. Insulin is the most important regulator of glucose homeostasis.
Major Risk Factors for Hyperglycemia
- Weight more than 120% of the desired body weight
- Family history of type 2 diabetes
- Native Americans, Hispanics, Asian Americans, Pacific Islanders, or African Americans
- Presence of hyperlipidemia or hypertension
- History of gestational diabetes
- Presence of polycystic ovarian syndrome
Epidemiology
The incidence of hyperglycemia has increased dramatically over the last two decades due to increased obesity, decreased activity level, and an aging population. The prevalence is equal between men and women. The countries with the greatest number of patients with diabetes included China, India, United States, Brazil, and Russia. Hyperglycemia is more prominent in low to medium-income households.
The latest data released by the Centers for Disease Control and Prevention indicate that there are nearly 30.5 million Americans with diabetes and nearly 84 million Americans with prediabetes. These numbers are set to increase significantly over the next decade.
Pathophysiology
Hyperglycemia in a patient with type 1 diabetes is a result of genetic, environmental, and immunologic factors. These lead to the destruction of pancreatic beta cells and insulin deficiency. In a patient with type 2 diabetes, insulin resistance and abnormal insulin secretion lead to hyperglycemia.
According to recent studies, metabolic disturbances like type 2 diabetes mellitus increases the risk of cognitive decline and Alzheimer dementia. Alzheimer dementia is also a risk factor for diabetes type 2. Recent studies have indicated these diseases are connected both at clinical and molecular levels. Like peripheral insulin resistance leading to type 2 diabetes, brain insulin resistance is linked to neuronal dysfunction and cognitive impairment in Alzheimer dementia.
History and Physical
Symptoms of severe hyperglycemia include polyuria, polydipsia, and weight loss. As the patient’s blood glucose increases, neurologic symptoms can develop. The patient may experience lethargy, focal neurologic deficits, or altered mental status. The patient can progress to a comatose state. Patients with diabetic ketoacidosis may present with nausea, vomiting, and abdominal pain in addition to the above symptoms. They also may have a fruity odor to their breath and have rapid shallow respirations, reflecting compensatory hyperventilation for the acidosis.
Diabetic Ketoacidosis
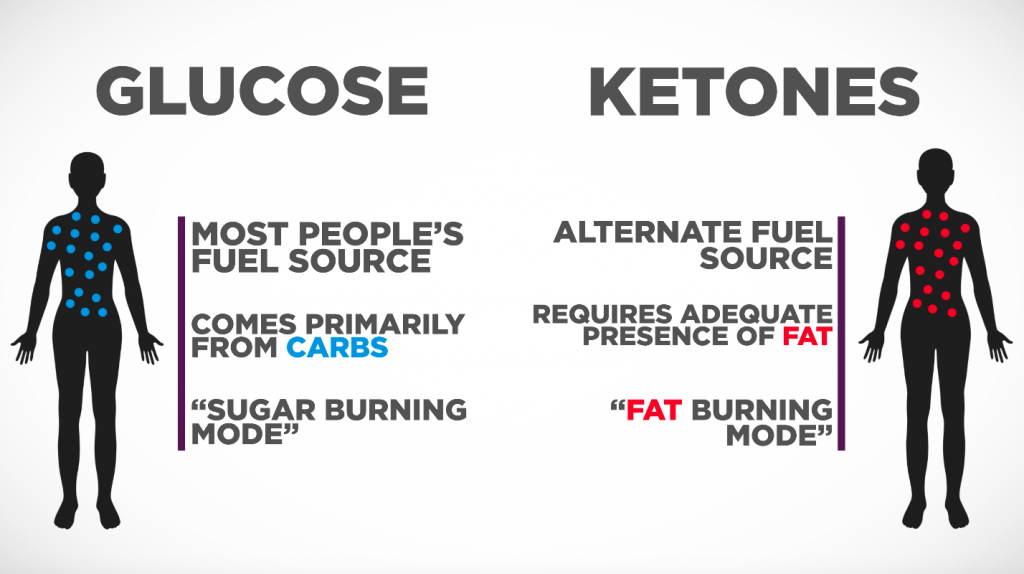
Ketosis is a metabolic state characterized by elevated levels of ketone bodies in the blood or urine. Physiological ketosis is a normal response to low glucose availability, such as low-carbohydrate diets or fasting, that provides an additional energy source for the brain in the form of ketones. In physiological ketosis, ketones in the blood are elevated above baseline levels, but the body’s acid–base homeostasis is maintained. This contrasts with ketoacidosis, an uncontrolled production of ketones that occurs in pathologic states and causes a metabolic acidosis, which is a medical emergency.
Diabetic ketoacidosis (DKA) is a life-threatening problem that affects people with diabetes. It occurs when the body starts breaking down fat at a rate that is much too fast. The liver processes the fat into a fuel called ketones, which causes the blood to become acidic.
Causes
DKA happens when the signal from insulin in the body is so low that:
- Glucose (blood sugar) can’t go into cells to be used as a fuel source.
- The liver makes a huge amount of blood sugar.
- Fat is broken down too rapidly for the body to process.
The fat is broken down by the liver into a fuel called ketones. Ketones are normally produced by the liver when the body breaks down fat after it has been a long time since your last meal. These ketones are normally used by the muscles and the heart. When ketones are produced too quickly and build up in the blood, they can be toxic by making the blood acidic. This condition is known as ketoacidosis.
DKA is sometimes the first sign of type 1 diabetes in people who have not yet been diagnosed. It can also occur in someone who has already been diagnosed with type 1 diabetes. Infection, injury, a serious illness, missing doses of insulin shots, or the stress of surgery can lead to DKA in people with type 1 diabetes.
People with type 2 diabetes can also develop DKA, but it is less common and less severe. It is usually triggered by prolonged uncontrolled blood sugar, missing doses of medicines, or a severe illness or infection.
Symptoms
The three main symptoms of diabetic ketoacidosis are polyuria (excessive urination), polydipsia (excessive thirst), and polyphagia (excessive hunger). The excessive thirst and urination are responsible for the impressive level of dehydration these patients will often present.
Common symptoms of DKA can include:
- Decreased alertness
- Deep, rapid breathing
- Dehydration
- Dry skin and mouth
- Flushed face
- Frequent urination or thirst that lasts for a day or more
- Fruity-smelling breath
- Headache
- Muscle stiffness or aches
- Nausea and vomiting
- Stomach pain
Pediatric Hyperglycemia
Juvenile diabetes is an extremely tough condition for the patient and family. Juvenile diabetics usually require insulin. Pediatric hyperglycemia can present with or without ketosis and their blood glucose levels can be so high that they can’t be measured accurately with a glucometer. Pediatric hyperglycemic patients are prone to seizures and dehydration. Some juvenile diabetics are undiagnosed, this horrible condition could be the undiscovered cause of the medics next call.
