Getting SPASTIC With Pediatric Altered Mental Status
Published .
What is altered mental status?
Altered mental status (AMS) is a disruption in how your brain works that causes a change in behavior. This change can happen suddenly or over days. AMS ranges from slight confusion to total disorientation and increased sleepiness to coma.
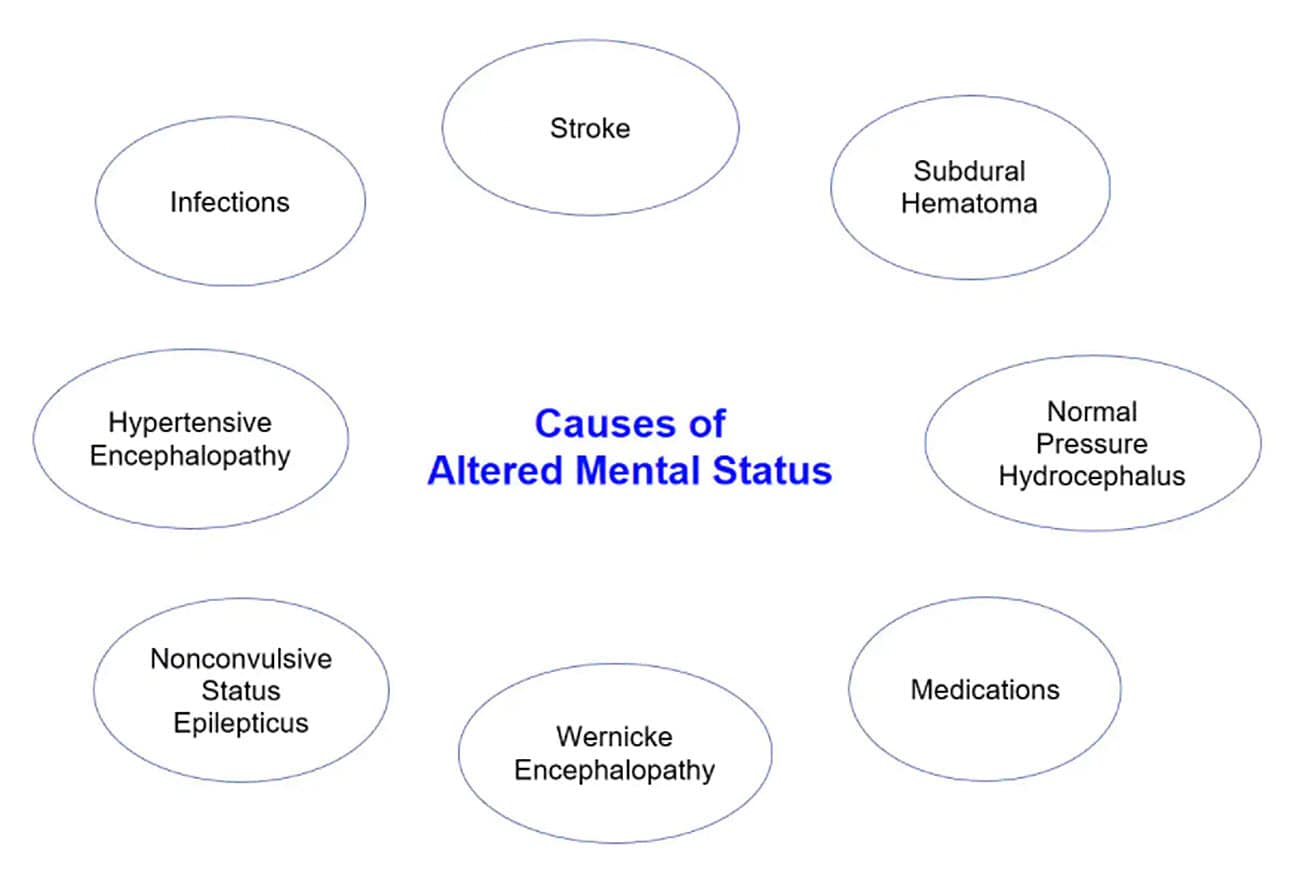
What causes AMS?
AMS can be caused by physical, psychological, and environmental factors. In older adults, AMS may be caused by a combination of these factors. The following are some of the most common causes of AMS:
- Diseases or conditions in the body that can affect your brain and nervous system:
- Hypoxia (low oxygen levels)
- Low or high blood sugar levels, or diabetic ketoacidosis
- Heart attack
- Dehydration, low or high blood sodium levels
- Thyroid or adrenal gland disease
- Urinary tract infection or renal failure
- Diseases or conditions within your skull:
- Seizures
- Head traumas, concussions
- Brain tumors or strokes
- Brain disease, such as encephalopathy
- High altitude cerebral edema (brain tissue swelling at high altitude)
- Other factors:
- Burns
- Hypothermia (low body temperature), hyperthermia (high body temperature), or heat stroke
- Toxic plants, such as mushrooms
- Carbon monoxide
- Drug or alcohol withdrawal
- Psychiatric problems
Time to round up the usual suspects
Nearly every cause of altered mental status has a definitive test. When the ambulance crew assesses a patient with altered mental status, they will not have the advantage of a myriad of clinical tests. What the ambulance crew needs is an easy way to assess common causes of altered mental status. When the patient is conscious, the ambulance crew should use the SPASTIC pneumonic:
Sugar – Check patients blood glucose level
Poisons – Inquire about the possibility of poisoning
Alcohol – Do the rescuers smell alcohol?
Stroke – Could the patient be having a stroke
Trauma – Is there a history of a head injury?
Infection – Is the patient running a fever?
Crack or other drugs – Is the patient on drugs?
Pediatric Causes Of Altered Mental Status
Pediatric patients generally do not have strokes, but they do have seizures. Seizures can be the result of a fever (febrile seizure). A febrile seizure can result from something as simple as an ear infection. If the infant or child is experiencing a first time seizure, the medics really need to figure out the underlying cause (with the SPASTIC pneumonic). Infants can have non convulsive seizures that result in periods of apnea. These non convulsive seizures often lead to cardiac arrest. As always, initial management of all patients are guided by the primary survey.
What about when the patient is unresponsive?
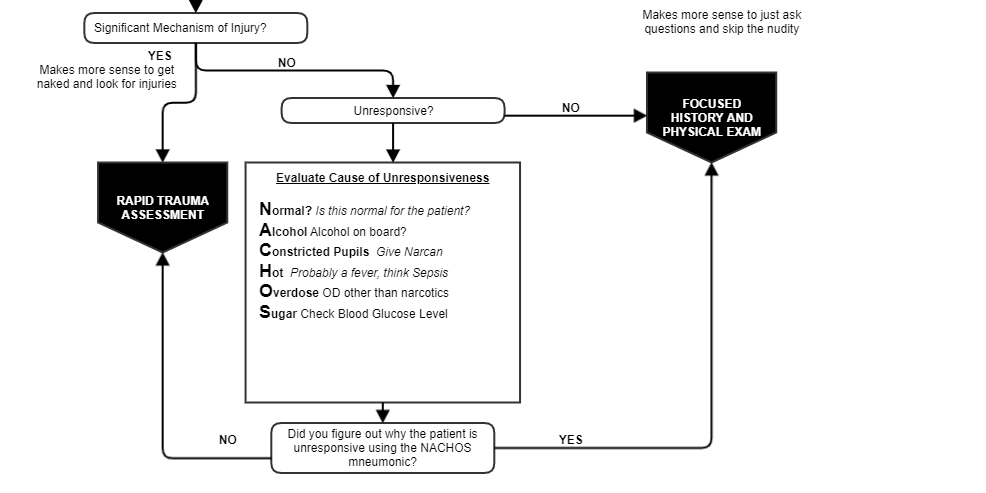
The problem with unresponsive patients is that there is always the possibility that they were injured with a mechanism of injury the responders can’t readily identify. If only the medics had some idea of why the patient is unresponsive. If the medics knew why the patient was unresponsive there would be no reason to look for injuries. If the medics are having to decide whether they should cut the clothes off an unresponsive to look for injuries or not, they should use the NACHOS pneumonic.

Normal – Is this behavior normal for the patient. Perhaps this is completely normal behavior after the patient has experienced a seizure.
Alcohol – Does the patient smell like alcohol?
Constricted pupils – Are the patient’s pupils constricted? This usually means narcotic overdose. Perhaps it’s time for some Narcan.
Hot – Does the patient’s skin feel hot or does the patient seem febrile with a contact free thermometer?
Otherwise overdose – Look for partially chewed up pills or empty pill bottles.
Sugar – Check the patient’s blood glucose level
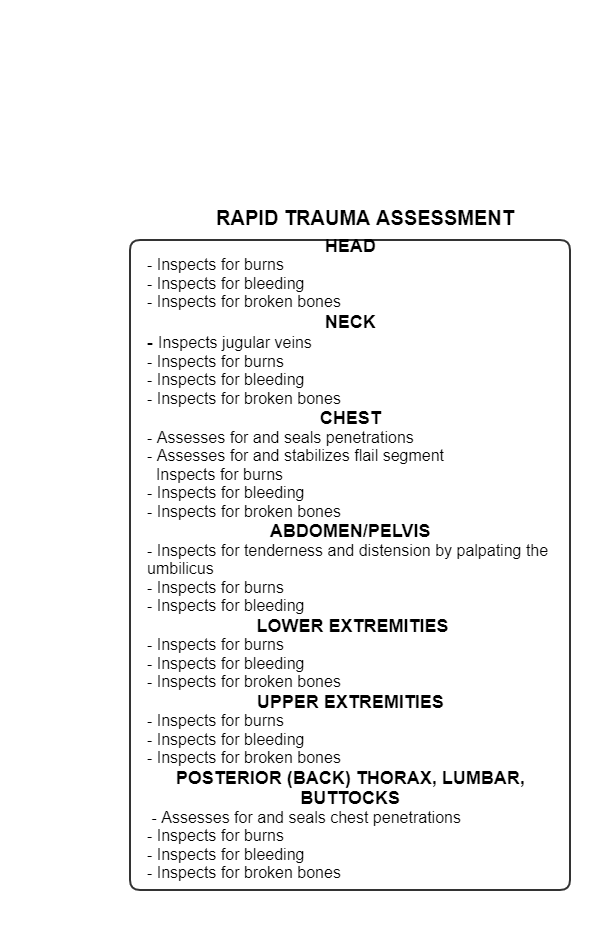
If the medics find the patient is unresponsive for one of these reasons, the search is over. However, if the medics fail to find the explanation they want with NACHOS, it’s time to look for injuries with the rapid trauma assessment.