The Secondary Survey
Published (updated: ).
The Context Of The Secondary Survey
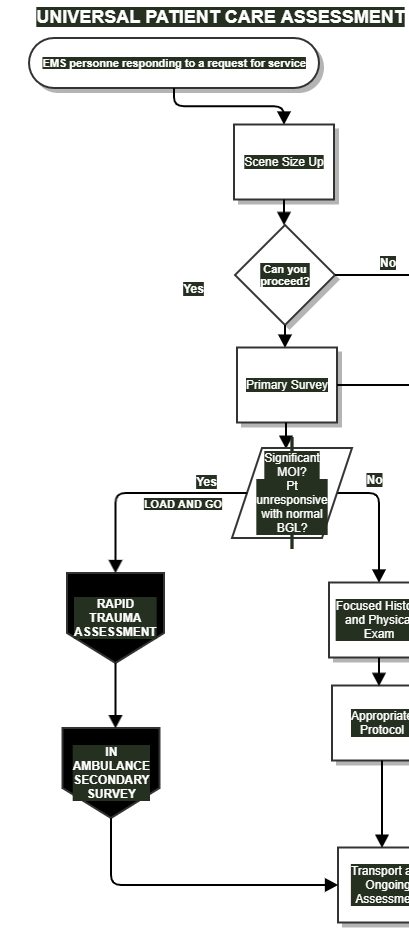
After the medics have assessed the patient for burns bleeding and broken bones, they package the patient. While enroute to the hospital, the medics job is not over. There is another assessment to perform while they are underway: The In Ambulance Secondary Survey
The In Ambulance Secondary Survey follows the rapid trauma assessment. The assessment is performed after the patient is loaded in the ambulance. The assessment is not intended for all patients and is primarily intended for trauma patients and patient’s who are unresponsive for unknown reasons (NACHOS negative).
The sequence of events follows the work flow of any call. Obtain patient information and vital signs then call the hospital and give a radio report. If there are multiple medics in the back of the ambulance, all of these tasks could be performed simultaneously. So what are the medics to do while enroute to the emergency department? They look from head to toe looking for more specific injuries. The georgiaemsacademy head to toe survey was developed to be conclusive enough to provide enough information that, when properly trained, will allow medics could see injuries that are not visible to the eye. The world of trauma looks so much different when the unseen is visible and the role of the medic becomes so much more valuable than just giving the patient a ride to the hospital.
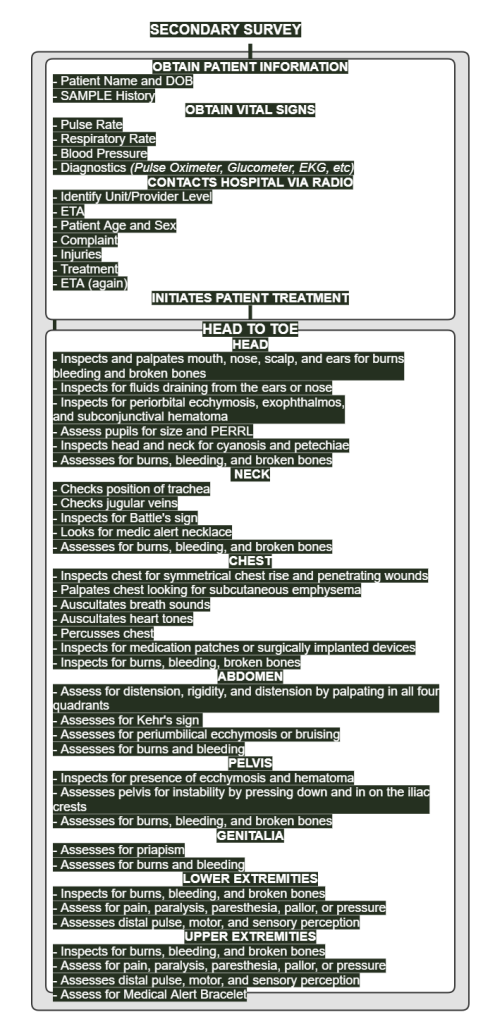
Start By Obtaining Patient History, Vital Signs, and Contact The Hospital
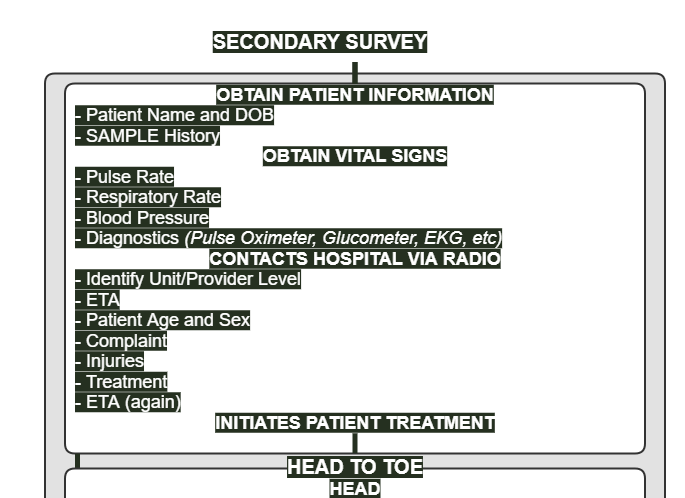
Obtaining the patient’s name and DOB is more important than most medics can appreciate. Hospitals don’t really like to treat patient’s when they don’t even know the patient’s name or date of birth (it’s kind of hard to enter them into the patient database without some basic information).

Go through the SAMPLE history as much as time will allow. Obviously, since the medics are treating a trauma patient, the onset of symptoms will be sudden. Notwithstanding obvious answers, the information in the SAMPLE history could be really important to the patient, considering the fact that the patient may require emergency surgery. Surgeons loathe emergency surgery. Most surgeons like to ensure the patient is prepped for surgery and nothing in the gastrointestinal tract. (not to mention shaving the pubes). Think about how little the surgeons would appreciate the patient having a bowel movement while in surgery.
Vital signs are taken every 5 to 15 minutes. The rationale is two fold: the medics need to see if their interventions are helping and the data will be useful later when doctors want to see if the patient is getting better or worse (trending). The easiest way to accomplish this trending vital sign measurement is with a non invasive blood pressure machine.
The emergency department staff is not fond of surprises. Depending upon what the medics find wrong with the patient, the emergency department may need special equipment or even special physicians. The following constitutes minimal information for a radio report (and less is always more over the radio) and is in the appropriate order:
- Identify Unit/Provider Level
- ETA (estimated time of arrival)
- Patient Age and Sex
- Complaint
- Injuries
- Treatment
- ETA (again)
After the call to the emergency has been completed, the medics should take a few minutes to initiate any treatment that they wanted to initiate before, but for the sake of time chose to do it enroute to the hospital. This is where the medics may opt to give medication or start an IV. Traction splinting can be performed in the back of the ambulance for the same reason.
HEAD TO TOE
HEAD



- Inspects and palpates mouth, nose, scalp, and ears for burns bleeding and broken bones
- Inspects for fluids draining from the ears or nose
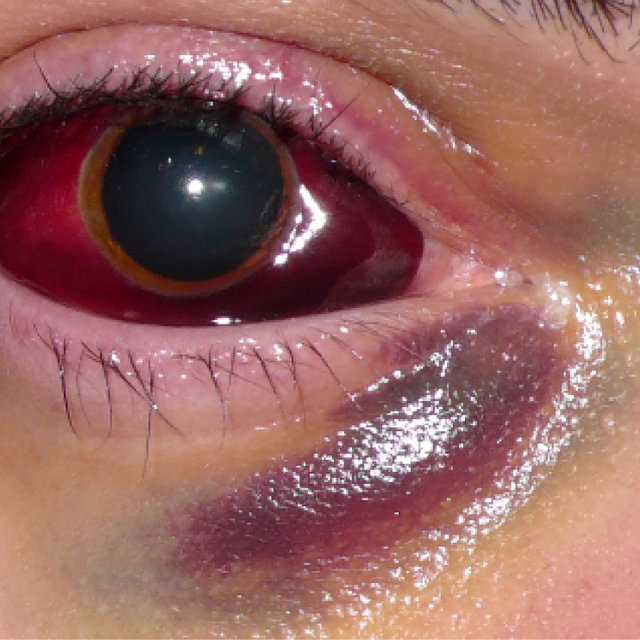
- Inspects for periorbital ecchymosis, exophthalmos, and subconjunctival hematoma
- Assess pupils for size and PERRL
- Inspects head and neck for cyanosis and petechiae
- Assesses for burns, bleeding, and broken bones
Fluids draining out of the mouth, nose, or ear could be blood, or could be blood mixed with cerebrospinal fluid. Cerebrospinal fluid (CSF) leaks are one of the common complications after traumatic brain injuries (TBI). The risks of CSF leaks can be detrimental to the outcomes of the patients. Early diagnosis and proper management is imperative for it is strongly associated with a better long-term prognosis of the patients. Diagnostic tools for CSF leaks are still under debate. Nevertheless, many reports of successful treatments for CSF leaks have been published with introduction of various repair techniques for leakage sites even though it is surgically challenging. CSF leaks are strongly suggest a basilar skull fracture (which is a fracture of the base of the skull).
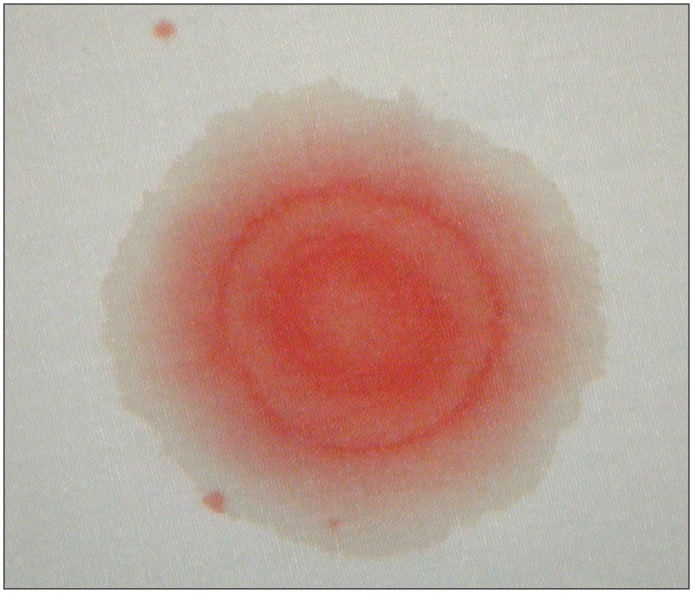
Looking at how the blood stains the sheets or 4 x 4’s, one can see a halo around the drop of blood. This is highly suggestive of CSF leakage. Another (less accurate) measure is to assess the blood glucose level of the blood from the ear and nose

Periorbital ecchymosis (Racoon’s eyes) and Battle’s sign are also signs of a basilar skull fracture. The base of the skull is near the ears. Anytime there is a broken bone, there will be bleeding. The blood can collect around the eyes (periorbital ecchymosis) and behind the ears (Battle’s sign).
Exophthalmos is bulging or protruding eyeballs. This is often caused by strangulation the result of a heavy object falling on the chest (traumatic asphyxia). Exophthalmos from traumatic asphyxia would be likely to be found with cyanosis and petechiae (purplish rash from busted capillaries under the skin). Exophthalmos is more commonly found due to Graves disease (or hyperthyroidism) than traumatic asphyxia.
Unequal pupils is a sign of a head injury. A finding of unequal pupils could mean a closed head injury with increased intracranial pressure. The finding is also associated with cranial nerve damage sustained from the force of impact. To assess the pupils, the patient should be loaded in the back of the ambulance with the lights turned off.
- Instruct the patient to look at the ceiling of the ambulance (turn the bright ceilings off, but leave the other lights on).
- Observe the size and shape of the pupils (they should be round and equal in size). Estimate the size based on the pupil size chart.
- Turn on the penlight and shine it directly into the patient’s right eye at a distance of approximately 3 inches from the eye.
- Observe the pupil size quickly decrease (constrict) in both eyes.
- Move the penlight away from the eyes.
- Observe the increased size of both pupils (dilate) after the penlight is moved away.
- Shine the penlight directly into the child’s left eye at a distance of approximately 3 inches from the eye.
- Observe the pupil size quickly decrease (constrict) in both eyes.
- Shine the penlight into the right eye and observe the pupil size (it should stay small).
- In a smooth motion, swing the penlight (still on) to the left eye and observe the pupil size (it should stay small).
NECK

- Checks position of trachea
- Checks jugular veins
- Inspects for Battle’s sign
- Looks for medic alert necklace
- Assesses for burns, bleeding, and broken bones
The jugular veins are assessed while on scene while performing the rapid trauma assessment. A finding of jugular vein distention means that the patient probably has an injury in the chest (which may or may not visible just by looking at the chest). A finding of tracheal deviation only means one thing, the patient has a tension pneumothorax. This late finding means the patient requires immediate needle chest decompression or will quickly die. Tracheal deviation sounds like it would be easy to see, but the trachea would have to shift a considerable distance to be visible making it hard to spot.
CHEST

- Inspects chest for symmetrical chest rise and penetrating wounds
- Palpates chest looking for subcutaneous emphysema
- Auscultates breath sounds
- Auscultates heart tones
- Percusses chest
- Inspects for medication patches or surgically implanted devices
- Inspects for burns, bleeding, broken bones
Anytime there is a pneumothorax (a hole in the lung) air will escape under skin causing subcutaneous emphysema. Subcutaneous emphysema generally can’t be seen, but it can be felt. All the medics have to do is palpate the skin of the chest and under the arms to feel for small pockets of air that are often described as bubble wrap.
The medics should have found any penetrating wounds or flail segments while on scene, but if they didn’t, they will surely have much easier time seeing the injury thanks to the generous lighting in the back of the ambulance. A penetrating wound should be sealed with an occlusive dressing and a flail chest stabilized with a large bulky dressing.
Assessing breath sounds at this juncture are intended to listen for unequal chest rise. The finding of unequal chest rise is associated with a pneumothorax. Since the stethoscope is out, the medic next listen to heart tones. The medics are listening for muffled heart tones. The finding of a muffled heart tone is associated with a pericardial tamponade (bleeding in the pericardial sac that could affect blood flow if not treated soon). The finding is also associated with infections of the pericardium (pericarditis).
ABDOMEN

- Assess for tenderness, rigidity, and distension by palpating in all four quadrants
- Assesses for Kehr’s sign
- Assesses for periumbilical ecchymosis or bruising
- Assesses for burns and bleeding
In the rapid trauma assessment, the medics would have assessed for distention and/or rigidity in the hopes of explaining a patient’s shock. In the ambulance, the medics should assess for tenderness. Tenderness is pain upon palpation (conscious patients only). If the pain complains of shoulder pain when palpating the abdomen, the patient has Kehr’s sign. Kehr’s sign means the patient may have a ruptured hollow organ (presumably a spleen). Inspection of the the umbilicus revealing ecchymosis or bruising is another sign of internal bleeding.
PELVIS
- Inspects for presence of ecchymosis and hematoma
- Assesses pelvis for instability by pressing down and in on the iliac crests
- Assesses for burns, bleeding, and broken bones
GENITALIA
- Assesses for priapism
- Assesses for burns and bleeding
LOWER EXTREMITIES
- Inspects for burns, bleeding, and broken bones
- Assess for pain, paralysis, paresthesia, pallor, or pressure
- Assesses distal pulse, motor, and sensory perception
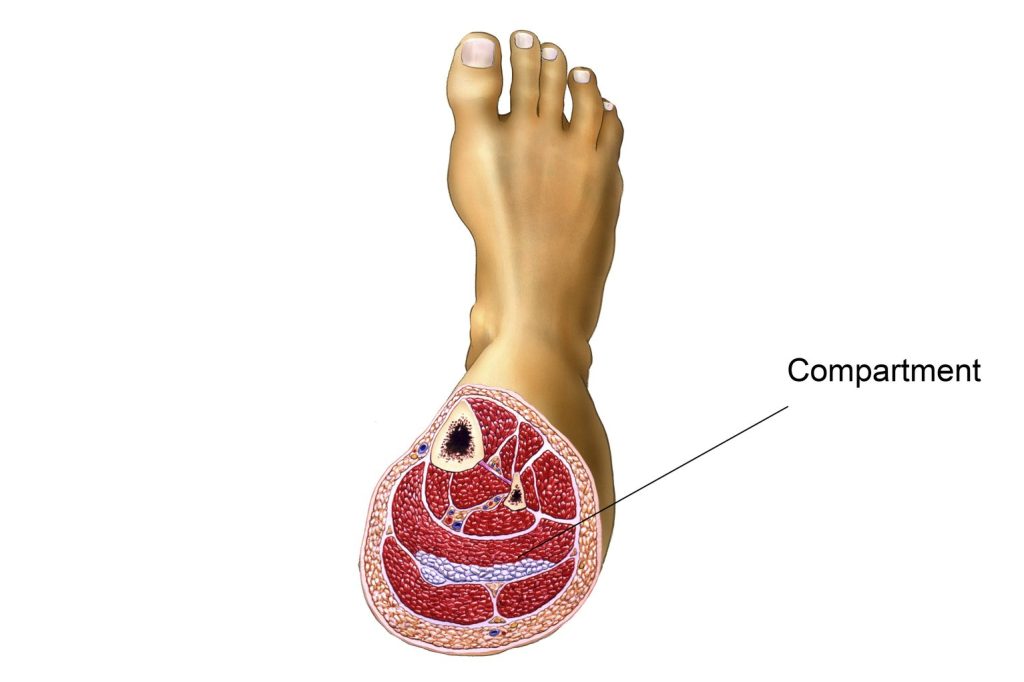
Assessing and documenting deficits of distal pulse, motor, and sensory perception can reveal telling clues about a spinal cord injury (conscious patients of course). As the medics move down the leg and look for injuries, they should be on the lookout for pain, paralysis, paresthesia, pallor, or pressure in the lower extremities. The finding of pain, paralysis, paresthesia, pallor, or pressure could mean compartment syndrome. Acute compartment syndrome can be caused by blunt force trauma that doesn’t break any bones. Bleeding is occurring in one of four different ‘compartments’ in the structure of the muscles of the leg (or arm for that matter). The patient will be in a lot of pain as the injury probably feels like a tourniquet. Since there is no obvious injury, compartment syndrome is often undiagnosed in the emergency department. As a result, amputation is sometimes the cure. If the doctors can figure this out (with the help of the medics), a procedure called a fasciotomy can be performed to restore circulation to the leg.
UPPER EXTREMITIES
- Inspects for burns, bleeding, and broken bones
- Assess for pain, paralysis, paresthesia, pallor, or pressure
- Assesses distal pulse, motor, and sensory perception
- Assess for Medical Alert Bracelet
