The Cardiovascular Exam
Published (updated: ).
Taking A Closer Look At Vital Signs

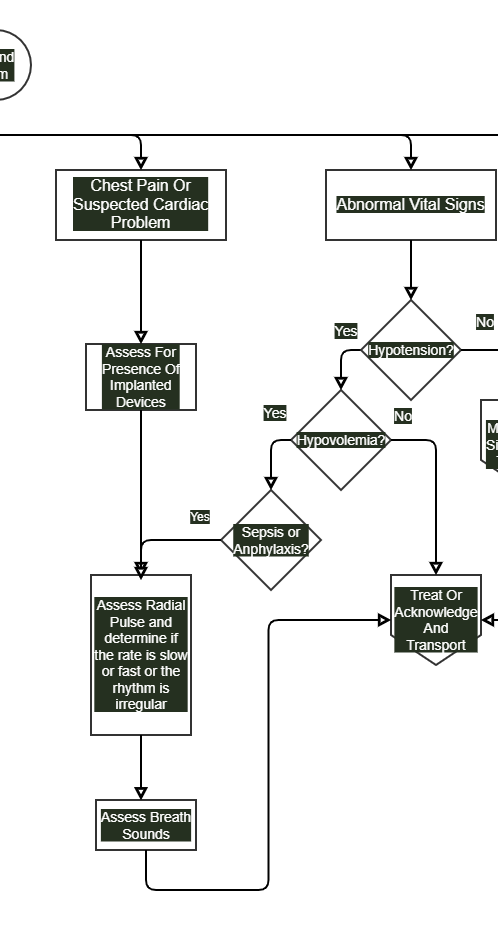
When the patient is complaining of chest pain or their complaint causes the medics to consider a cardiovascular cause of the patient’s complaint, the focused physical exam must address the possibility of cardiac dysrhythmias. A cardiac dysrhythmia is an irregularity in the patient’s heart rhythm. A very common form of dysrhythmia is atrial fibrillation which results in a very irregular heart beat. An irregular heart rate is discovered when the medics assess the radial pulse. The medics should look for the following:
- Rapid Heart Rate – A resting heart rate that is greater than 120 beats per minute could mean the patient is experiencing a tachycardia.
- Slow Heart Rate – A slow heart rate could be a sign that the patient is experiencing a symptomatic bradycardia. A bradycardia is typically evaluated when the patient’s heart rate is less than 60. There are many people who have a heart rate less than 60 and it’s not the job of EMS to screen the public looking for asymptomatic bradycardias. The real value of discovering a patient with a bradycardia is when the patient is symptomatic or even unresponsive.
- Irregular Heart Rate – There are many cardiac dysrhythmias that result in an irregular heart rate. When assessing the heart rate, determine the regularity of the rhythm. Cardiac rhythms can either be regular, irregularly regular (irregular at regular intervals), or irregularly irregular (irregular at irregular intervals).
Evaluating Blood Pressure
Hypertension by itself is not an situation that EMS has any business treating. Hypertension is treated medically, but done over days, months, or years. Further, hypertensive patients are generally very stable and will maintain or improve while enroute to the hospital without much concern by the medics.
Hypotension is a serious cause of concern due to it’s ability to transcend into shock. Further, careless movement could result in the patient deteriorating, possibly to the point of respiratory or cardiac arrest. Hypotensive patients may quickly require blood transfusions or aggressive medical treatment once they arrive at the hospital. The emergency department can be just as clueless as the general public at determining the underlying cause of shock. When the medics discover hypotension, immediate treatment and further investigation is required. The first suspect is blood or other fluid loss. Inquiring about events preceding the complaint will reveal details such as exposure to hot climate, gastrointestinal bleeding, or medical or surgical procedure gone wrong. If fluid loss can’t be found in the history, the history could point to an infection leading to sepsis or anaphylaxis. Perhaps the patient is experiencing a cardiac dysrhythmia that is leading to the hypotension. Determining the rate, rhythm, and regularity of the radial (or carotid) pulse could reveal a cardiac origin of the patient’s hypotension.
Listening To Breath Sounds
Auscultation of the chest may reveal adventitious breath sounds. Listening for crackles or wheezing may reveal clues as to the nature of the patient’s chest pain.
Putting It All Together