Respiratory Exam
Published (updated: ).
Easily Assess The Patient’s Respiratory Complaint And Figure Out The Underlying Condition
Let’s be honest, is it really that difficult to just go to somebody’s house and with very little effort determine they are having shortness of breath? And if all the medics did was give some oxygen and transport to the hospital, that would probably be a reasonable enough response on the vast majority of difficulty breathing calls. As acceptable a practice as this is, the medics could do a much better job.
Believe it or not, a patient with shortness of breath is by far the most unstable patient transported in an ambulance. The likelihood that the patient with respiratory distress will decompensate and require positive pressure ventilation or CPR is significantly higher than trauma patients with gunshot wounds or multiple system trauma. The truth is the patient that is most likely to not make it to the hospital is that patient with chronic obstructive pulmonary disease (COPD) or congestive heart failure (CHF).
Respiratory distress, like shock, comes in three phases:
- Respiratory Distress – This phase, the patient is experiencing shortness of breath. The patient is able to compensate for their respiratory distress by increasing their respiratory rate. Administering oxygen makes the job of breathing easier for the patient. Administering oxygen and transport is all that is required for these very uncomplicated patients.
- Respiratory Compromise – In this phase, the patient is no longer compensating for their respiratory distress. The patient is demonstrating accessory muscle usage (intercostal and clavicular retractions, nasal flaring, positioning, not able to speak in complete sentences). The patient is using more oxygen than they are taking in, and is only hanging in there due to the body’s amazing ability to store oxygen in red blood cells and even bone marrow. This patient needs more than just supplemental oxygen. This patient desperately needs the medics to identify the underlying cause of their shortness of breath and specifically treat that problem (with a specific intervention). Further, this patient will probably require at least an overnight stay at the hospital to monitor the patient and ensure their oxygenation is caught up prior to discharge.
- Respiratory Failure – In this phase, the patient has lost the battle with their respiratory condition. The patient will present with altered mental status and probably require positive pressure ventilation. The worst thing the medics can do is lay the patient supine and ventilate. Ventilation can be performed while the patient is sitting in the fowlers position (assuming the patient was sitting in that position when they stopped breathing).
Inspect The Chest
When inspecting the chest, assess for chest rise and symmetry. Does the chest appear to rise adequately? Next look for signs of accessory muscle usage. By seeing the accessory muscle use, the medics can understand which phase of respiratory distress the patient is in. Sometimes, the patient’s problem can be discovered just by looking at the chest. Perhaps the patient has a broken rib or even an impaled object on the chest.

Auscultate Breath Sounds
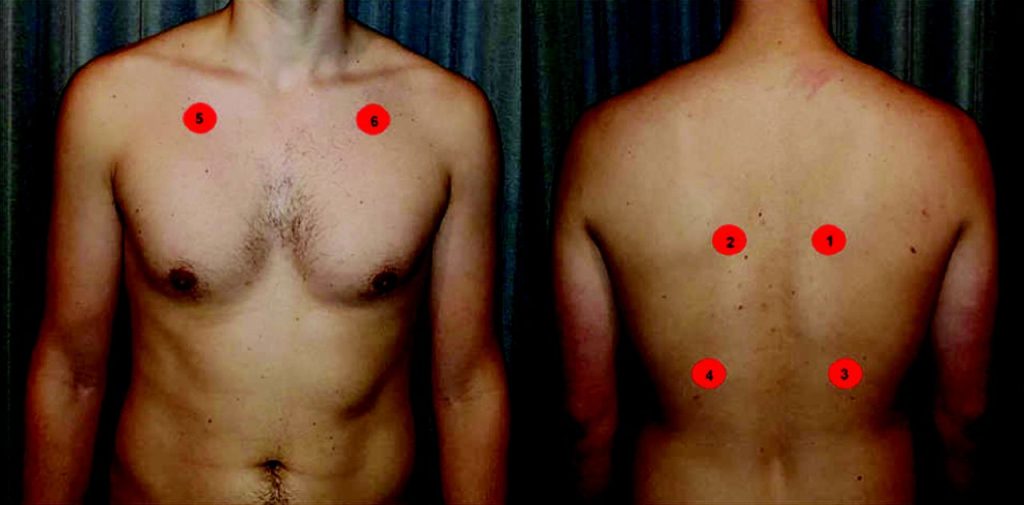
By listening for adventitious breath sounds, the medics can get an idea of what is wrong with the patient’s lungs. The medics can auscultate the lung fields with their stethoscope on the locations on the patients chest (see above). Auscultation of breath sounds can be taught in a way that is significantly more comprehensive than above, however, the medics only need to get a basic ‘theme’ or overall sound. It is possible to hear more than one breath sound The basic sounds are crackles, wheezing, and clear. Stridor is a sound that doesn’t require a stethoscope to hear.
Crackles are the sounds of fluids moving through the alveoli. The term crackles is often referred to as rales and/or rhonchi. When a patient has crackles, this could mean they have congestive heart failure or pneumonia (2 very different conditions with same breath sound).
Wheezes are the sound of bronchoconstriction. The patient’s bronchioles have constricted or narrowed, generally making it difficult for the patient to exhale. The sound is a high pitched, almost musical sounding tone. Another feature of the sound is the short inspiratory phase and prolonged expiratory phase. By estimating the inspiratory to ventilatory phase ratio, the medics could classify the patient’s asthma or COPD as minor (1:2), moderate (1:3) or severe (1:4). Many times, wheezing can be heard without a stethoscope. Conditions that typically present with wheezing include asthma, emphysema (COPD), and anaphylaxis.
Normal breath sounds sound unobstructed and the inspiratory to expiratory phase ratio is 1:1. Just because the medics do not hear any adventitious breath sounds doesn’t mean they can’t pinpoint the cause of the patient’s respiratory distress.
Put It All Together
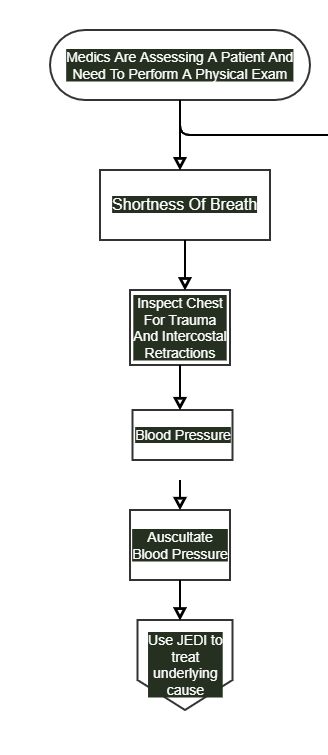
Figure Out The Underlying Cause Compare Breath Sounds And Vital Signs
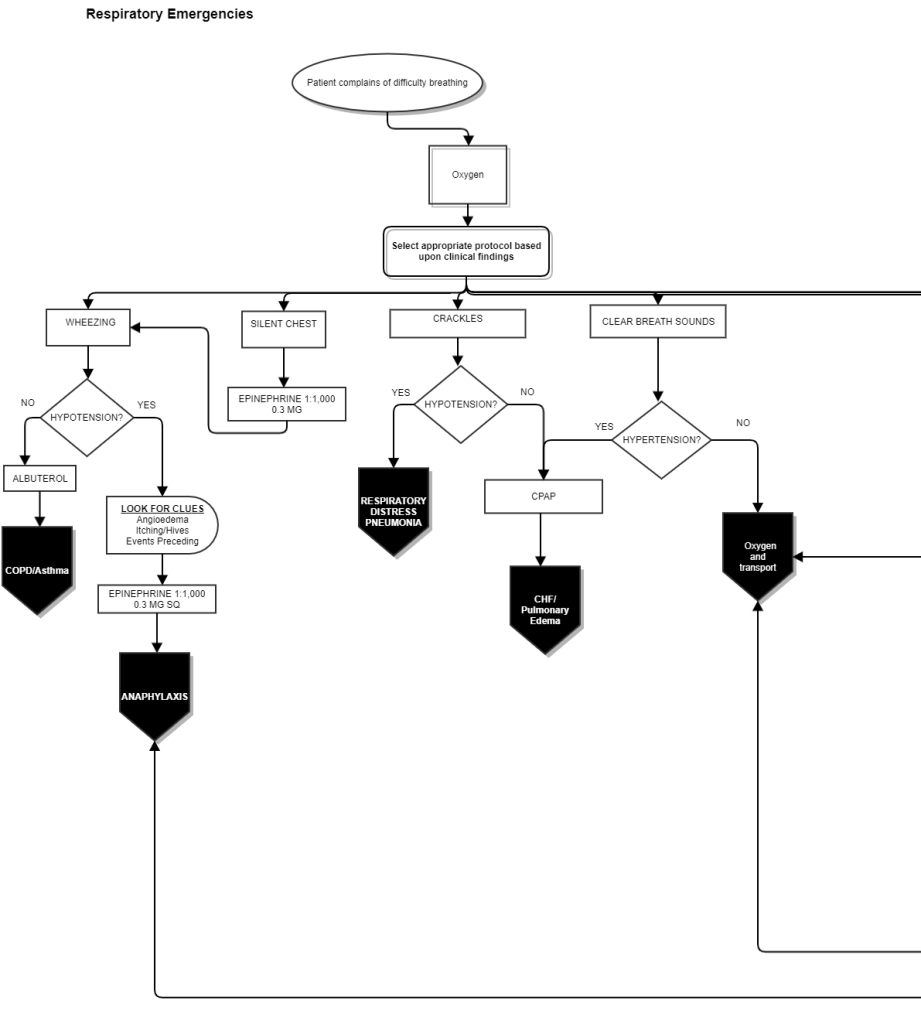
If you look at the flowchart, you can see some specific patterns based around the breath sounds. The pattern is complete when the medics factor in the blood pressure. Hypotension is more or less a relative term which could mean the patient is in shock or has a lower than normal blood pressure (think 100mm/Hg systolic on 200 pound patient, no way that guy walks around with that blood pressure). Hypertension is a relative term as well. Hypertension in this case could mean 200 mm/Hg systolic or it could mean 160 mm/Hg systolic. Whatever it is, it’s not 120/80.
Cases Of Wheezing
Wheezing is not uncommon for all the respiratory conditions covered in the flowchart, however, if the predominant sound is wheezing then it’s just wheezing. If the patient’s blood pressure is hypotensive, then medics are looking at anaphylaxis. If the patient is not hypotensive (meaning it’s not hypotensive but could be normal or even hypertensive), the medics are probably dealing with COPD-emphysema or asthma. Anaphylaxis and Asthma or COPD are treated differently. Being able to differentiate is key when treating the patient who really needs the medics to start dialing in on the problem in lieu of just transporting with oxygen.
Cases Of Crackles
If the predominant sound is crackles the medics could be looking at pneumonia or congestive heart failure (CHF). The most common is pneumonia but CHF is always out there and has the potential to give the medics the wildest ride to the hospital yet. Again, the key to differentiating is the blood pressure. If the blood pressure is hypotensive, the patient is probably suffering from pneumonia (or something like pneumonia like RSV). If the patient is hypertensive (and this case greater than 140 mm/Hg), the patient is probably experiencing congestive heart failure (CHF). CHF and pneumonia (and all things like pneumonia) are treated differently. Being able to differentiate is key when treating the patient who really needs the medics to start dialing in on the problem in lieu of just transporting with oxygen
Cases Of Normal Breath Sounds
Just because the breath sounds are normal doesn’t mean that there is nothing wrong or the medics won’t be able to discern the nature of the problem. If the patient is hypertensive, the patient is probably experiencing congestive heart failure (CHF). If the patient is not hypotensive, the medics really have nowhere to go with this simple assessment. Going back to the SAMPLE history may lead the medics to greater understanding the nature of the patient’s problem.
