Setting The Stage For Obtaining A Patient History
Published (updated: ).
Setting The Stage
The patient doesn’t have the privilege of checking out the ambulance crew on the internet before they arrive. They are stuck with who they get (the same can be said for medics). Given the realities of responding to incidents, the patient may have had to wait a considerable time. Despite the fact that everybody thinks they are entitled to a response that is 8 minutes or less, the trip to the patient’s house may have taken a considerably longer period of time. Since perfection in terms of customer service is probably not going to happen, the medics would be wise to do the following:
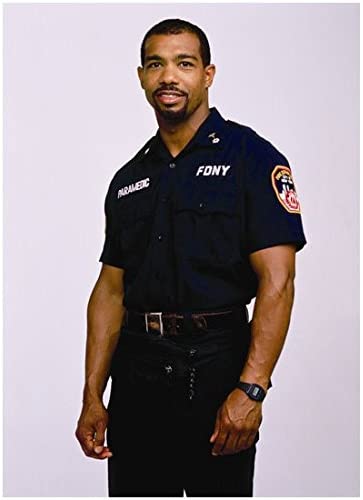
- Wear a clean and pressed uniform. Looking sharp in uniform is a type of resume. The patient will judge the medics based solely on their appearance. Look the part.
- Bring equipment to the patient. The public expects the medics to be prepared for anything. Walking in the door with a jump bag or stretcher is akin to an attorney walking into a meeting carrying a briefcase (even if there is nothing in it).
- Be courteous. Being courteous can simply mean greeting the patient or family with the greeting of the day. It’s okay to be quiet. Nobody understands the life of a medic, so the patient or family would be the last to understand why the medics are in a bad mood. Try to leave it at the door.
- Focus on the patient. The medics are at the scene to serve the patient. Even if the medics don’t really care about the patient, going through the SAMPLE history at least has the potential of leading the patient to think otherwise.
- Get on the patients level – If the patient is laying in bed or on a sofa, standing over the patient and talking down to them is not going to make the patient feel that the medics want to hear about the patient’s problems. Sit down, even if it’s on the floor.
- Respect the patient’s personal space.
- Refer to the patient as mister, missus, or miss unless the patient wants you to call them by their first name.
- Avoid calling patients ‘honey’ or ‘granny’. The use of such familiar terms are inappropriate in emergency situations.
- When the patient says something, write it down. The patient has no idea what is being written, but they will assume it’s in response to what they are saying. The public expects EMS to listen to their problems even if they can’t solve them.
If The Medics Want To Sleep Tonight, Maybe They Should Learn About The Present Illness
Many times, EMS responds to patient’s with chronic medical problems. Diabetes, seizures, angina, asthma, and psychiatric problems generally can’t be resolved by a singular trip to the emergency department. Before the patient’s problem is resolved (if it gets resolved), there may be many trips to the emergency room via ambulance. So what is the chief complaint when it’s a chronic problem? The chief complaint IS the chronic problem. But instead of asking what is wrong, the medics are asking what is wrong TODAY. When did the problem get so bad that the patient felt like they needed to call 911. Once the medics understand the events that preceded the 911 call, then the reason why the patient requested an ambulance to the scene becomes more obvious. Patients with chronic medical problems call 911 for a variety of reasons, but mostly for the following:
- The hospital discharged the patient after instructing the patient to contact their primary care physician. The problem the is that the primary care physician is either not available for 3 more months or never existed in the first place.
- The hospital discharged the patient with a prescription. The patient, for whatever reason, was unable to obtain the medication and needs to be taken back to the emergency room so they can get some medication.
- The patient has a serious chronic medical or psychiatric condition and also a domestic situation that is unstable and volatile. Had the domestic situation been stable, there would have been no need for EMS in the first place.
- The patient is addicted to narcotics or other medicine and generally calls 911 for transportation to the emergency department to get their fix.
- It’s just hot outside and there is no air conditioning.
Inquiring about the present illness should lead to follow-up questions that seek to find individual factors that could have resulting in the patient’s condition deteriorating. Medications not being filled, tobacco use, alcohol or drug abuse and diet can result in a patient’s condition that is only getting worse. Some patients are just hungry because they have no money for food. Perhaps the patient is a victim of domestic abuse or someone is stealing their medications.
So Why Am I Here?
Don’t fall into the trap of assuming that the complaint is as it was when it was dispatched. The public is plagued with a lack of ability to communicate their needs over the phone. In person is where the real complaint can be revealed. The medics should ask open ended questions. An open ended question is a question that can’t be answered with yes or no. The easiest question and most open ended question of all time is, “…So, why am I here?”
Encourage the patient to continue explaining their problem by writing everything down. All Patients love to be listened to. Additionally, gestures such as nodding, or occasionally telling the patient, “I’m listening.” will encourage the patient to continue explaining their problem. This is referred to as facilitation.
Another clue that tells the patient that you are listening to their problem is by repeating the patient’s words in an attempt to gain additional responses. These responses will help the medics clarify any ambiguous statements or words. When the medics are reflecting the patient’s words back to the patient, they should feel free to articulate the feelings expressed by the patient during their ordeal (empathetic response). If the patient’s feelings are completely unfounded, the medics may want to confront the patient (obviously in a respectful manner). The medics may need to interpret the patient’s words into their own words. This is not only helpful in the eyes of the patient (who is convinced the medics are listening to their problems) but can also be useful when the the English language itself is a barrier to communication.
