A Complete Guide To Pulse Oximetry
Published (updated: ).
At georgiaemsacademy, we teach that patients who are not alert may need positive pressure ventilation and that patients with rapid respiratory rate or demonstrated work of breathing need oxygen via non rebreather mask. It’s easy to keep things that simple if you are primarily looking at ventilation as all one has to do is count respiratory rate. But ventilation is only one side of the coin. The other side of the coin is oxygenation. Could a patient have normal respirations and still by hypoxic?
Ventilation and oxygenation are distinct but interdependent physiological processes. While ventilation can be thought of as the delivery system that presents oxygen-rich air to the alveoli, oxygenation is the process of delivering O2 from the alveoli to the tissues in order to maintain cellular activity. Further, oxygenation can refer to the removal of carbon dioxide from the cells. Can a patient’s ventilation be measured by oxygenation? In some cases yes. Doctors use a range of tests to determine how well a patient is ventilating and different tests are used to determine oxygenation. What can medics observe about a patient that will give them clues about oxygenation?
- Cyanosis – Blue discoloration of the skin
- Pallor – Extremely pale or white skin
- Mottling – Skin with purple discolorations
What would a patient with normal oxygenation look like (besides normal)?
- Normal skin color
- Normal oral mucosa (The oral mucosa is the mucous membrane lining or “skin” inside of the mouth, including cheeks and lips)
Probably The Most Misunderstood Device Of EMS
Pulse oximeters measure oxygenation. They don’t measure ventilation. This is the source of the confusion. Pulse oximeter have become a vital sign of sorts, given the data they collect on the patient (pulse rate and blood saturation of oxygens). Pulse oximeters were intended to be used on the ambulance as a patient monitoring device. A patient monitoring device is used to keep an eye on a patient during transport in the event that the medics become distracted. If the patient begins to decompensate, the machine sounds an alarm, causing the medics to spring into action.
But they do actually measure oxygenation. What if the medics through their index of suspicion considered the possibility that the patient has latent (hidden) hypoxia. The pulse oximeter could be useful as a focused physical exam.
Recommendations for Health Care Providers
- Be aware that multiple factors can affect the accuracy of a pulse oximeter reading, such as poor circulation, skin pigmentation, skin thickness, skin temperature, current tobacco use, and use of fingernail polish.
- Refer to the device labeling or the manufacturer’s website to understand the accuracy of a particular brand of pulse oximeter and sensor. Different brands of pulse oximeters and even different sensors (finger clip versus adhesive) may have a different accuracy level. Pulse oximeters are least accurate when oxygen saturations are less than 80%.
- Consider accuracy limitations when using the pulse oximeter to assist in diagnosis and treatment decisions.
- Use pulse oximeter readings as an estimate of blood oxygen saturation. For example, a pulse oximeter saturation of 90% may represent an arterial blood saturation of 86-94%.
- When possible, make diagnosis and treatment decisions based on trends in pulse oximeter readings over time, rather than absolute thresholds.
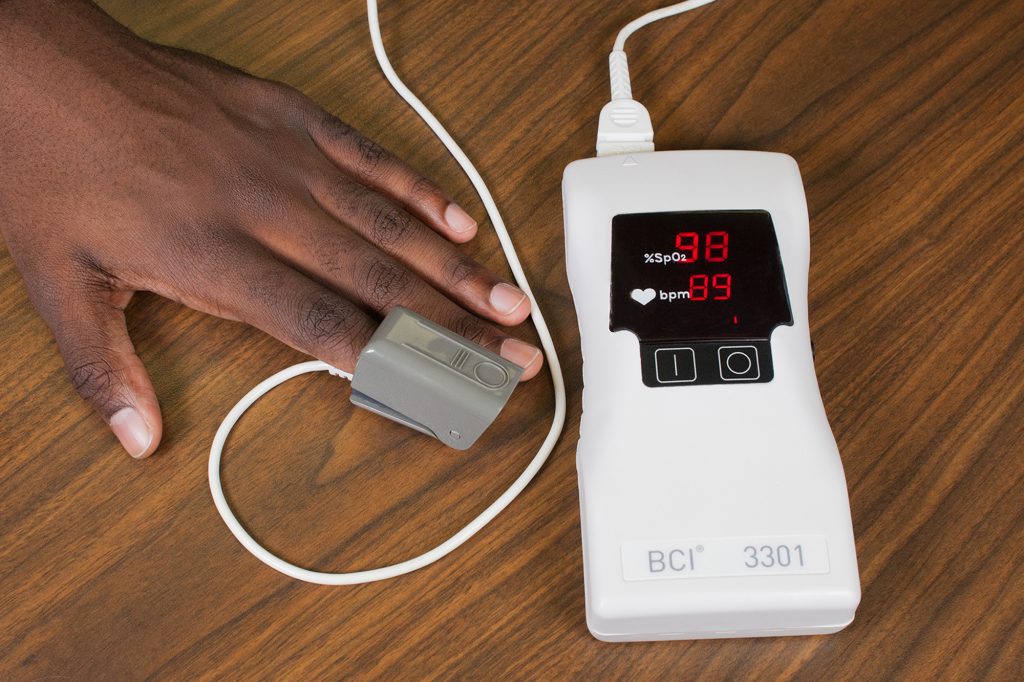
A pulse oximeter is a device that is usually placed on a fingertip. It uses light beams to estimate the oxygen saturation of the blood and the pulse rate. Oxygen saturation gives information about the amount of oxygen carried in the blood. The pulse oximeter can estimate the amount of oxygen in the blood without having to draw a blood sample.
Most pulse oximeters show two or three numbers. The most important number, oxygen saturation level, is usually abbreviated SpO2, and is presented as a percentage. The pulse rate (similar to heart rate) is abbreviated PR, and sometimes there is a third number for strength of the signal. Oxygen saturation values are between 95% and 100% for most healthy individuals, but sometimes can be lower in people with lung problems. Oxygen saturation levels are also generally slightly lower for those living at higher altitudes.
There are two categories of pulse oximeters: prescription use and over the counter (OTC).
- Prescription oximeters are reviewed by the FDA, receive 510(k) clearance, and are available only with a prescription. The FDA requires that these pulse oximeters undergo clinical testing to confirm their accuracy. They are most often used in hospitals and doctors’ offices, although they may sometimes be prescribed for home use.
- Over-the-counter (OTC) oximeters are sold directly to consumers in stores or online and include smart phone apps developed for the purpose of estimating oxygen saturation. Use of OTC oximeters has increased as a result of the COVID-19 pandemic. These products are sold as either general wellness or sporting/aviation products that are not intended for medical purposes, so they do not undergo FDA review. OTC oximeters are not cleared by the FDA and should not be used for medical purposes.
Interpretation and Limitations of Pulse Oximetry
Pulse oximeters have limitations and a risk of inaccuracy under certain circumstances. In many cases, the level of inaccuracy may be small and not clinically meaningful; however, there is a risk that an inaccurate measurement may result in unrecognized low oxygen saturation levels. Therefore, it is important to understand the limitations of pulse oximetry and how accuracy is calculated and interpreted.
FDA-cleared prescription pulse oximeters are required to have a minimum average (mean) accuracy that is demonstrated by desaturation studies done on healthy patients. This testing compares the pulse oximeter saturation readings to arterial blood gas saturation readings for values between 70-100%. The typical accuracy (reported as Accuracy Root Mean Square or Arms) of recently FDA-cleared pulse oximeters is within 2 to 3% of arterial blood gas values. This generally means that during testing, about 66% of SpO2 values were within 2 or 3% of blood gas values and about 95% of SpO2 values were within 4 to 6% of blood gas values, respectively.
However, real-world accuracy may differ from accuracy in the lab setting. While reported accuracy is an average of all patients in the test sample, there are individual variations among patients. The SpO2 reading should always be considered an estimate of oxygen saturation. For example, if an FDA-cleared pulse oximeter reads 90%, then the true oxygen saturation in the blood is generally between 86-94%. Pulse oximeter accuracy is highest at saturations of 90-100%, intermediate at 80-90%, and lowest below 80%. Due to accuracy limitations at the individual level, SpO2 provides more utility for trends over time instead of absolute thresholds. Additionally, the FDA only reviews the accuracy of prescription use oximeters, not OTC oximeters meant for general wellness or sporting/aviation purposes.
How It Works
A typical pulse oximeter uses an electronic processor and a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient’s body, usually a fingertip or an earlobe. One LED is red, with wavelength of 660 nm, and the other is infrared with a wavelength of 940 nm. Absorption of light at these wavelengths differs significantly between blood loaded with oxygen and blood lacking oxygen. Oxygenated hemoglobin absorbs more infrared light and allows more red light to pass through. Deoxygenated hemoglobin allows more infrared light to pass through and absorbs more red light. The LEDs sequence through their cycle of one on, then the other, then both off about thirty times per second which allows the photodiode to respond to the red and infrared light separately and also adjust for the ambient light baseline.
The amount of light that is transmitted (in other words, that is not absorbed) is measured, and separate normalized signals are produced for each wavelength. These signals fluctuate in time because the amount of arterial blood that is present increases (literally pulses) with each heartbeat. By subtracting the minimum transmitted light from the transmitted light in each wavelength, the effects of other tissues are corrected for, generating a continuous signal for pulsatile arterial blood.

