Dying Doesn’t Always Come Easy
Published (updated: ).
With Hypoxia, The Cell Goes To Plan B
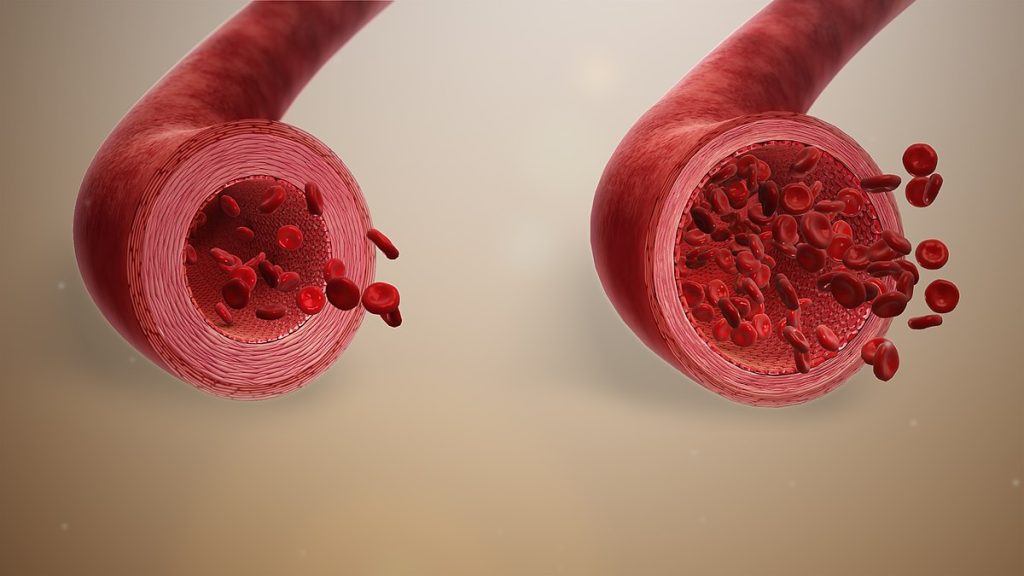
Hypoxia is a physiological cue that impacts diverse physiological processes, including energy metabolism, autophagy, cell motility, angiogenesis, and erythropoiesis. One of the key cell-autonomous effects of hypoxia is as a modulator of cell proliferation. For most cell types, hypoxia induces decreased cell proliferation, since an increased number of cells, with a consequent increase in O2 demand, would only exacerbate hypoxic stress. However, certain cell populations maintain cell proliferation in the face of hypoxia. This is a common pathological hallmark of cancers, but can also serve a physiological function, as in the maintenance of stem cell populations that reside in a hypoxic niche.
The production of energy requires oxygen. The electron transport chain, where the majority of ATP is formed, requires a large input of oxygen. However, many organisms have developed strategies to carry out metabolism without oxygen, or can switch from aerobic to anaerobic cell respiration when oxygen is scarce.
During cellular respiration, some living systems use an organic molecule as the final electron acceptor. Processes that use an organic molecule to regenerate NAD+ from NADH are collectively referred to as fermentation. In contrast, some living systems use an inorganic molecule as a final electron acceptor. Both methods are called anaerobic cellular respiration, where organisms convert energy for their use in the absence of oxygen.
The fermentation method used by animals and certain bacteria (like those in yogurt) is called lactic acid fermentation. This type of fermentation is used routinely in mammalian red blood cells and in skeletal muscle that has an insufficient oxygen supply to allow aerobic respiration to continue (that is, in muscles used to the point of fatigue). The excess amount of lactate in those muscles is what causes the burning sensation in your legs while running. This pain is a signal to rest the overworked muscles so they can recover. In these muscles, lactic acid accumulation must be removed by the blood circulation and the lactate brought to the liver for further metabolism.
Hypoglycemia
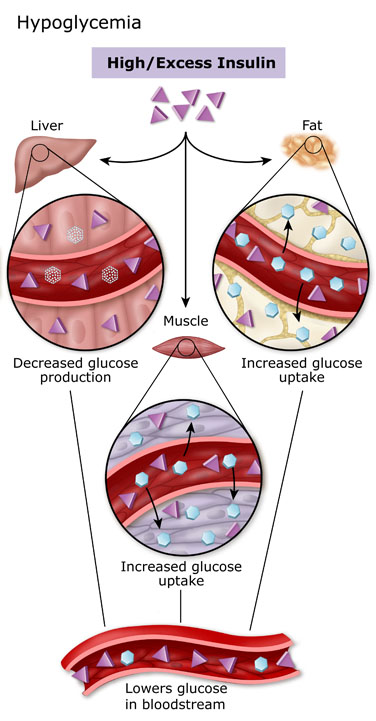
Hypoglycemia is often defined by a plasma glucose concentration below 70 mg/dL; however, signs and symptoms may not occur until plasma glucose concentrations drop below 55 mg/dL. The symptoms of Whipple’s triad have been used to describe hypoglycemia since 1938. For the Whipple triad, the practitioner must first recognize hypoglycemia symptoms, obtain low blood glucose, and finally, demonstrate immediate relief of symptoms by the correction of the low blood glucose after treatment.
The body has inherent counter-regulatory mechanisms to prevent hypoglycemic episodes. All of these counter-regulatory mechanisms include an interplay of hormones and neural signals to regulate the release of endogenous insulin, to increase hepatic glucose output, and to alter peripheral glucose utilization. Among the counter-regulatory mechanisms, the regulation of insulin production plays a major role. Decrease in insulin production as a response to low serum glucose isn’t the body’s first line of defense against hypoglycemia. For endogenous glucose production to take place, particularly hepatic glycogenolysis, low insulin levels are necessary. As plasma glucose levels decline, beta-cell secretion of insulin also decreases, leading to increased hepatic/renal gluconeogenesis and hepatic glycogenolysis. Glycogenolysis maintains serum glucose levels over 8 to 12 hours until glycogen stores are depleted. Over time, hepatic gluconeogenesis contributes more to maintaining euglycemia when required.
Infection
Infection does not necessarily lead to disease. Infection occurs when viruses, bacteria, or other microbes enter your body and begin to multiply. Disease, which typically happens in a small proportion of infected people, occurs when the cells in your body are damaged as a result of infection, and signs and symptoms of an illness appear.
In response to infection, your immune system springs into action. White blood cells, antibodies, and other mechanisms go to work to rid your body of the foreign invader. Indeed, many of the symptoms that make a person suffer during an infection—fever, malaise, headache, rash—result from the activities of the immune system trying to eliminate the infection from the body.
Pathogenic microbes challenge the immune system in many ways. Viruses make us sick by killing cells or disrupting cell function. Our bodies often respond with fever (heat inactivates many viruses), the secretion of a chemical called interferon (which blocks viruses from reproducing), or by marshaling the immune system’s antibodies and other cells to target the invader. Many bacteria make us sick the same way, but they also have other strategies at their disposal. Sometimes bacteria multiply so rapidly they crowd out host tissues and disrupt normal function. Sometimes they kill cells and tissues outright. Sometimes they make toxins that can paralyze, destroy cells’ metabolic machinery, or precipitate a massive immune reaction that is itself toxic.
Sepsis is the body’s extreme response to an infection. It is a life-threatening medical emergency. Sepsis happens when an infection you already have triggers a chain reaction throughout your body. Infections that lead to sepsis most often start in the lung, urinary tract, skin, or gastrointestinal tract. Without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death.
Infections can put you or your loved one at risk for sepsis. When germs get into a person’s body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Bacterial infections cause most cases of sepsis.
