Emergency Medications
Published (updated: ).
Medications EMT’s Can Administer
Aspirin

Nonprescription aspirin is used to prevent heart attacks in people who have had a heart attack in the past or who have angina (chest pain that occurs when the heart does not get enough oxygen). Nonprescription aspirin is also used to reduce the risk of death in people who are experiencing or who have recently experienced a heart attack. Nonprescription aspirin is also used to prevent ischemic strokes (strokes that occur when a blood clot blocks the flow of blood to the brain) or mini-strokes (strokes that occur when the flow of blood to the brain is blocked for a short time) in people who have had this type of stroke or mini-stroke in the past. Aspirin will not prevent hemorrhagic strokes (strokes caused by bleeding in the brain). Aspirin is in a group of medications called salicylates. It works by stopping the production of certain natural substances that cause fever, pain, swelling, and blood clots.
The adult dose of aspirin for chest pain is 325 mg or 4 baby aspirin. Baby aspirin was chosen because it can be chewed by the patient for faster digestion (not to mention they are delicious).
What are blood thinners?
Blood thinners are medicines that prevent blood clots from forming. They do not break up clots that you already have. But they can stop those clots from getting bigger. It’s important to treat blood clots, because clots in your blood vessels and heart can cause heart attacks, strokes, and blockages.
Who needs blood thinners?
- Certain heart or blood vessel diseases
- An abnormal heart rhythm called atrial fibrillation
- A heart valve replacement
- A risk of blood clots after surgery
- Congenital heart defects
- What are the different types of blood thinners?
There are different types of blood thinners:
Anticoagulants, such as heparin or warfarin (also called Coumadin), slow down your body’s process of making clots. Antiplatelets, such as aspirin and clopidogrel, prevent blood cells called platelets from clumping together to form a clot. Antiplatelets are mainly taken by people who have had a heart attack or stroke.
Oral Glucose
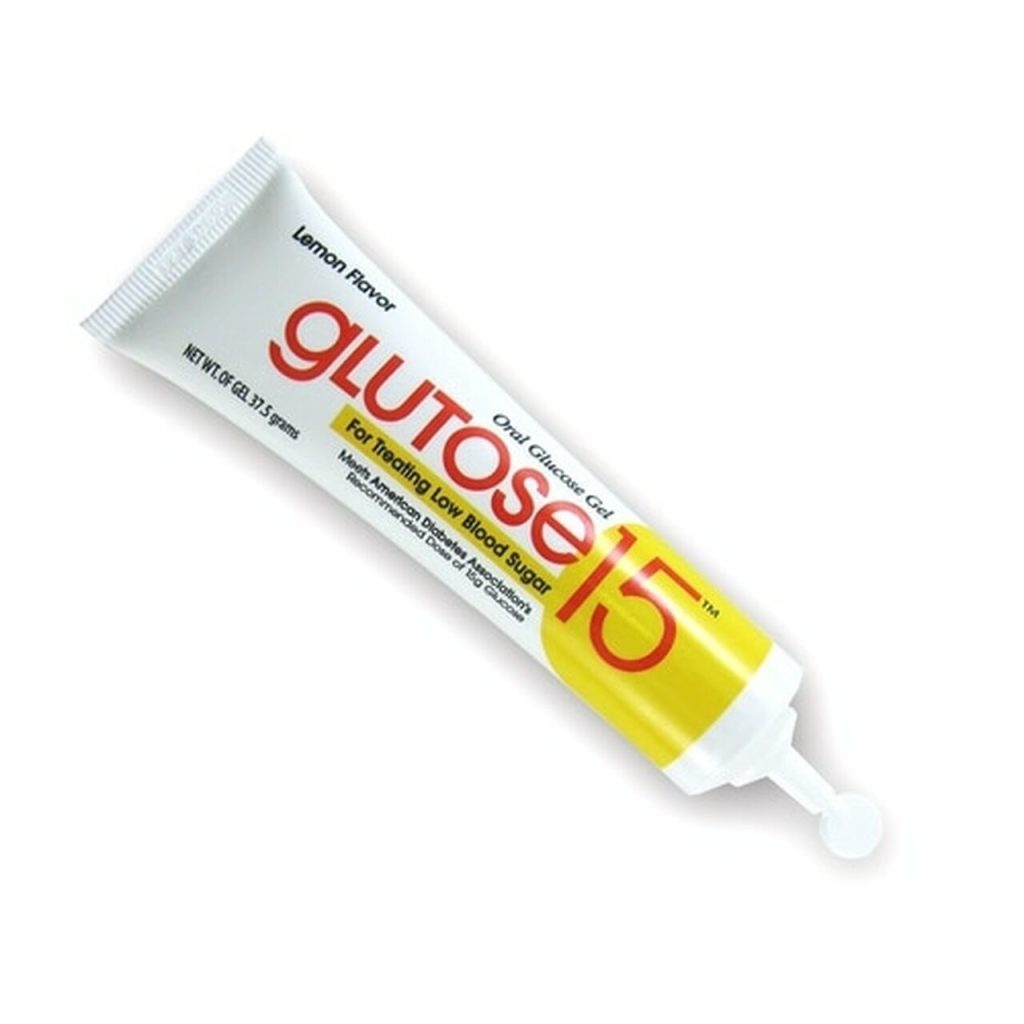
Oral glucose gel is an over-the-counter medication, consisting primarily of dextrose (sugar) and water, along with small amounts of other compounds. It is frequently used by people with diabetes and those with hypoglycemia to raise their blood glucose when it becomes dangerously low.
Hypoglycemia occurs when blood sugar levels drop too low; it can cause a variety of symptoms including hunger, sweating, rapid heart rate, and shaking. If left untreated, hypoglycemia can lead to a loss of consciousness. Onset of hypoglycemia can be sudden, requiring glucose levels to be normalized by consuming carbohydrates. Diabetics are generally recommended to carry 15 grams of glucose with them at all times. Oral glucose gel is used to raise dangerously low blood glucose concentration or blood glucose that has dropped too low for the person’s adaptive compensatory mechanisms to cope with. The gel may be self-administered or given by an Emergency Medical Technician or paramedic responding to a hypoglycemic emergency.
As glucose molecules will absorb directly through oral tissue, the gel is either swallowed directly or allowed to stay in the mouth momentarily to facilitate rapid absorption via various areas of the mouth cavity and then swallowed to allow absorption into the blood via the small intestine
Oxygen

Oxygen is an essential medicine used to care for patients at all levels of the healthcare system, including in surgery, trauma, heart failure, asthma, pneumonia and maternal and child care. Pneumonia alone accounts for 800 000 deaths per year. It is estimated that 20–40% of these deaths could be prevented with the availability of oxygen therapy.
Oxygen is a gas that your body needs to work properly. Your cells need oxygen to make energy. Your lungs absorb oxygen from the air you breathe. The oxygen enters your blood from your lungs and travels to your organs and body tissues. Certain medical conditions can cause your blood oxygen levels to be too low. Low blood oxygen may make you feel short of breath, tired, or confused. It can also damage your body. Oxygen therapy can help you get more oxygen.
What is oxygen therapy?
Oxygen therapy is a treatment that provides you with extra oxygen to breathe in. It is also called supplemental oxygen. It is only available through a prescription from your health care provider. You may get it in the hospital, another medical setting, or at home. Some people only need it for a short period of time. Others will need long-term oxygen therapy.
There are different types of devices that can give you oxygen. Some use tanks of liquid or gas oxygen. Others use an oxygen concentrator, which pulls oxygen out of the air. You will get the oxygen through a nose tube (cannula), a mask, or a tent. The extra oxygen is breathed in along with normal air.
There are portable versions of the tanks and oxygen concentrators. They can make it easier for you to move around while using your therapy.
Who needs oxygen therapy?
You may need oxygen therapy if you have a condition that causes low blood oxygen, such as:
- COPD (chronic obstructive pulmonary disease)
- Pneumonia
- COVID-19
- A severe asthma attack
- Late-stage heart failure
- Cystic fibrosis
- Sleep apnea
What are the risks of using oxygen therapy?
Oxygen therapy is generally safe, but it can cause side effects. They include a dry or bloody nose, tiredness, and morning headaches.
Oxygen poses a fire risk, so you should never smoke or use flammable materials when using oxygen. If you use oxygen tanks, make sure your tank is secured and stays upright. If it falls and cracks or the top breaks off, the tank can fly like a missile.
Activated Charcoal
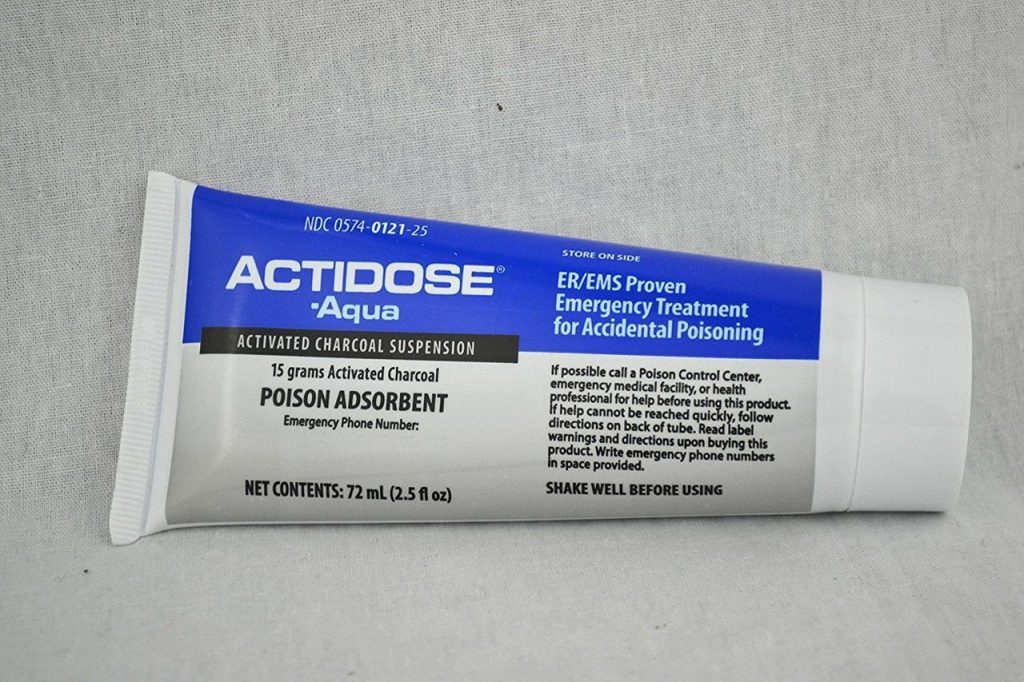
An oral suspension of activated charcoal should be considered in poisonings when gastrointestinal decontamination of an ingested toxin is indicated. Activated charcoal is most efficacious when given within one hour of ingestion of the toxin. Careful consideration of the contraindications should occur before treatment with activated charcoal.
Activated charcoal adsorbs ingested toxins within the gastrointestinal tract preventing the systemic absorption of that toxin. Activated charcoal only adsorbs toxins that are in the dissolved liquid phase via direct contact. Orally administered activated charcoal does not get absorbed through the gastrointestinal lumen and acts within the gastrointestinal (GI) tract in its unchanged form. Ingested toxins come in contact with activated charcoal if the drug has not yet been absorbed from the gastrointestinal lumen, or via recirculation of the toxin into the gut lumen by either enterohepatic recirculation, or entero-enteric recirculation through active secretion, or passive diffusion. Contraindications include:
- Patients with an unprotected airway (in other words, a depressed level of consciousness) without endotracheal intubation
- If activated charcoal use is likely to increase the risk and severity of aspiration of a toxin (hydrocarbons with high aspiration potentials)
- When the threat of GI perforation or hemorrhage is high secondary to medical conditions or recent surgery
- When endoscopy is likely to be attempted as activated charcoal may obscure endoscopic visualization
- In the presence of an intestinal obstruction
- When activated charcoal is known to not meaningfully adsorb the ingested toxin such as metals, acids, alkalis, electrolytes, or alcohols
Medications EMT’s can Assist with Administration
Inhaled bronchodilators

Bronchodilators are a type of medication that make breathing easier by relaxing the muscles in the lungs and widening the airways (bronchi). They’re often used to treat long-term conditions where the airways may become narrow and inflamed, such as: asthma, a common lung condition caused by inflammation of the airways.
Without spacer:
- Hold inhaler in dominant hand.
- Place mouthpiece in mouth with opening toward back of mouth, and have patient close lips around mouthpiece.
- Ask patient to inhale deeply and exhale completely.
- Ask patient to hold inhaler between thumb at the base and index and middle fingers at the top.
- Ask patient to tilt head back slightly and inhale deeply and slowly through mouth, while simultaneously depressing inhaler canister.
- Ask patient to hold breath for about 10 seconds without exhaling medication.
- Remove MDI while exhaling through nose or pursed lips.
With spacer:
- Insert MDI into end of spacer device.
- Ask patient to place spacer mouthpiece in mouth and close lips around mouthpiece, avoiding any exhalation openings on spacer.
- Ask patient to breathe regularly.
- Have patient depress medication canister to spray one puff into spacer device.
- Ask patient to breathe in deeply and slowly for about 5 seconds and to then hold breath at the end of inspiration for about 10 seconds.
- If one medication: have patient wait 20 to 30 seconds between inhalations
- If more than one medication: have patient wait 2 to 5 minutes between inhalations.
Epinephrine
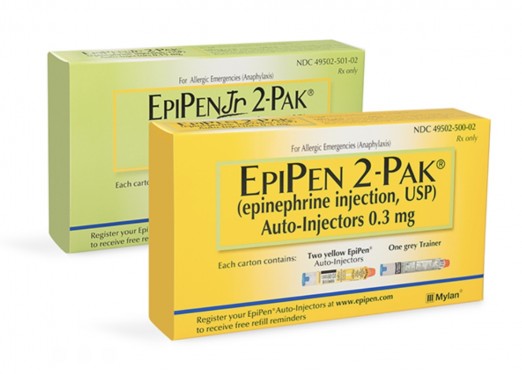
Epinephrine autoinjectors are hand-held devices carried by those who have severe allergies; the epinephrine delivered by the device is an emergency treatment for anaphylaxis.
When anaphylaxis is suspected, epinephrine solution should be given as soon as possible as an intramuscular injection, in the middle of the outer side of the thigh, which corresponds to the location of the vastus lateralis muscle. The injection may be repeated every 5 to 15 minutes if there is insufficient response. A second dose is needed in 16–35% of episodes with more than two doses rarely required; in around 80% of the cases where a second dose is administered, it is by a medical professional. It is not clear which are the people who might need a second injection at the outset. The intramuscular route is preferred over subcutaneous administration because the latter may have delayed absorption. Minor adverse effects from epinephrine include tremors, anxiety, headaches, and palpitations.
Nitroglycerin

Nitroglycerin sublingual tablets are used to treat episodes of angina (chest pain) in people who have coronary artery disease (narrowing of the blood vessels that supply blood to the heart). It is also used just before activities that may cause episodes of angina in order to prevent the angina from occurring. Nitroglycerin is in a class of medications called vasodilators. It works by relaxing the blood vessels so the heart does not need to work as hard and therefore does not need as much oxygen.
First, Take A Blood Pressure (Don’t administer if systolic BP is less than 130)
Nitroglycerin comes as a sublingual tablet to take under the tongue. The tablets is usually taken as needed, either 5 to 10 minutes before activities that may cause attacks of angina or at the first sign of an attack. Do not chew, crush, or swallow nitroglycerin sublingual tablets. Instead, place the tablet under your patient’s tongue or between your cheek and gum and wait for it to dissolve. The patient may feel burning or tingling in your mouth as the tablet dissolves. This is normal but is not a sign that the tablet is working. Do not be concerned that the tablet is not working if the patient does not feel the burning or tingling.
