Patient Assessment For Pediatric Patients
Published (updated: ).
The EMS crew should always be looking for a mechanism of injury, regardless of how a call is dispatched. In the case of the pediatric patient, mechanisms of injury may not be obvious. An infant falling off the countertop probably requires transport to a trauma center (fall twice the height of the infant). Broken furniture or a house that is in severe disrepair could also provide clues as to a hidden mechanism of injury. There could be abuse or even human trafficking occurring right in front of the medics eyes.
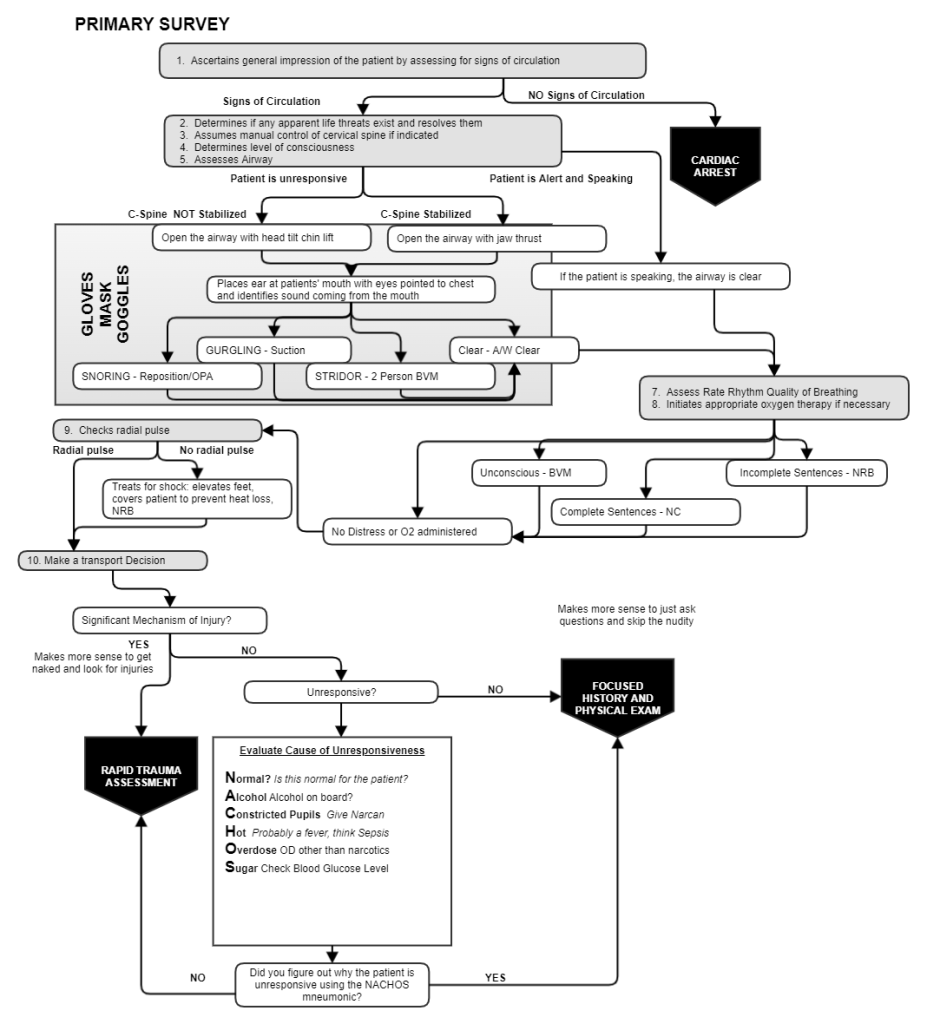
Initial management of all patients should be guided by the primary survey. The primary survey is the same for a pediatric patient as it is for an adult. Some differences that would apply to the infant or toddler:
- Supplemental oxygen – Despite the fact that ambulances carry pediatric oxygen masks, the patient may be too scared to wear a mask. In situations like this, blow-by oxygen can be administered. With blow-by oxygen, the mask is placed at the patient’s face and allowed to blow on the nose and mouth.
- Positive pressure ventilation given administered through a pediatric bag valve mask. Newborns, infants, and toddlers with a heartrate under 100 bpm are ventilated with a bag valve mask attached to oxygen (running at 15 lpm).
- CPR – The performance of CPR is age dependent and should always be performed by two rescuers. Neonatal (under 30 days old) receive 3 chest compressions for each ventilation. Infant receive CPR with 15 chest compressions and 2 ventilations. Toddlers and older children receive CPR at 30 chest compressions to 2 ventilations. Pediatric patients receive CPR for heart rates under 60 bpm.
- Assessment and treatment of shock – Pediatric patients with weak distal pulses are treated as shock patients. Shock is very dangerous for pediatric patients as their strange compensatory mechanisms lead to a sudden decompensation that often end in death. Capillary refill times of 3 seconds or greater should be viewed as shock and also treated as shock. Shock treatment is simple, prevent heat loss with a blanket, administer high flow oxygen, and elevate feet (if possible).

The SAMPLE history is a generic history taking method used by medics everywhere. The SAMPLE history should explain why EMS is with the patient. When the SAMPLE history doesn’t easily explain what is happening or why EMS was called in the first place, it’s time to ask more questions.
A history of fever and low activity level lends itself to an high index of suspicion for an infection. The same holds true for decreased appetite, thirst, and urine output. Pediatric patients probably spend about 25% of their life under the weather. Ebbs and tides in the patients developing immune system dictate that sometimes the patient is just going to be sick. Inquiring about bowel history normally wouldn’t be something that medics would ask about for an adult, but an infant that hasn’t had a bowel movement in several days is probably experiencing a bowel obstruction. History of nausea, vomiting, diarrhea or abdominal pain could lead the medics toward an index of suspicion of dehydration (which also leads to shock).
Generally speaking, infants and toddlers don’t have many drug allergies. But finding one that has a drug allergy and the medics are probably taking care of a chronically ill child. Chronically ill children often take numerous medications and complications from their condition. These complications and medications need to be inquired about and documented. If the medics are taking care of a chronically ill child, they should find out why the ambulance was requested.
Sometimes, ambulance crews encounter child abuse or poisoning. Subtle clues about abuse could be the relationship between the child and parents or evidence of healing from numerous injuries. Inconsistent stories from parents could indicate deception in the SAMPLE history. The SAMPLE history could lead to a discovery of a possible toxic ingestion. Perhaps the patient took some adult medication or drank a household chemical (especially toddlers).
