Exposure To Cold
Published .
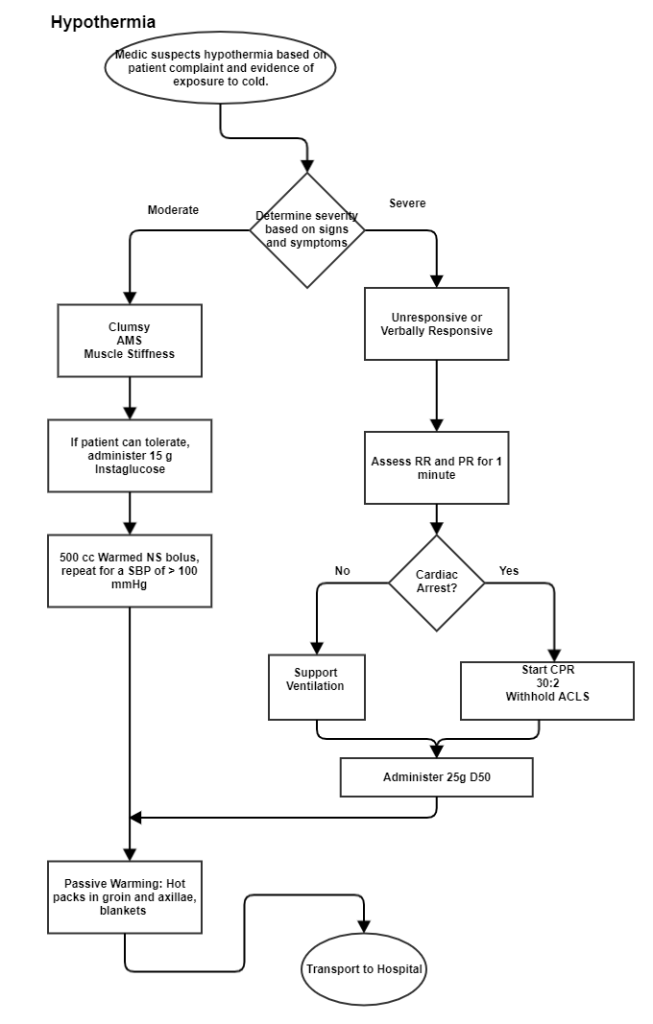
Hypothermia
When exposed to cold temperatures, the body begins to lose heat faster than it can be produced. Prolonged exposure to cold will eventually use up your body’s stored energy. The result is hypothermia, or abnormally low body temperature. A body temperature that is too low affects the brain, making the patient unable to think clearly or move well. This makes hypothermia particularly dangerous because a person may not know it is happening and will not be able to do anything about it.
It’s not just cold that can lead to hypothermia. Since water conducts heat better than air, the air doesn’t even have to be that cold in order to result in hypothermia. Wind results in heat loss by conduction. As air blows on the patient the heat is conducted into the air molecules then carried away. Pediatric and elderly patients struggle more with maintaining body temperature. In the case of the pediatric patient, their high body surface area to mass ratio sets them up for hypothermia. In other words, the amount of skin an infant or child has is greater in comparison to body weight than an adult. The elderly lose their body fat and their skin becomes paper thin (poor insulation from the environment). Various medical conditions such as diabetes, stroke, and heart disease can make it difficult for a patient to adapt to the temperature. Similarly, medications both medicinal and recreational (including alcohol) can affect how well a person can adapt to ambient temperatures.
Early Symptoms
- Shivering
- Fatigue
- Loss of coordination
- Poor judgement
- Complaints of joint/muscle stiffness
- Confusion and disorientation
Late Symptoms
- No shivering
- Stiff or rigid posture
- Blue skin
- Dilated pupils
- Slowed pulse and breathing
- Loss of consciousness
Initial management is based on the primary survey. With hypothermia, the heart rate will drop as low as the teens, so the medics should ensure they take a pulse for an entire minute. Hypothermic cardiac arrests can have good outcomes if CPR is performed adequately. Defibrillation with an AED can be used for a hypothermic cardiac arrest, however paramedics should minimize the medications they administer. Given the progression of symptoms, EMS providers may need to deduce that the patient’s problem is hypothermia. The SAMPLE history could reveal clues about the patient’s underlying illness, overdose, or poisoning. If the medics are concerned about hypothermia, palpating the abdomen with the back of a hand can provide a hint to the patient’s core body temperature (in this case, the abdomen would feel cold). The only accurate measurement of temperature is a core body temperature (rectal); any other measurement of temperature is just a guess.
Handle the patient with hypothermia very gently
- Move the patient into the warm ambulance.
- Remove their wet clothing.
- Warm the center of their body first-chest, neck, head, and groin-using an electric blanket, or hot packs if available; or use skin-to-skin contact under loose, dry layers of blankets, clothing, towels, or sheets.
- After their body temperature has increased, keep the victim dry and wrapped in a warm blanket, including the head and neck.
- If victim has no pulse, begin cardiopulmonary resuscitation (CPR).
Frostbite is a lot like a burn

Frostbite is an injury to the body that is caused by freezing. Frostbite causes a loss of feeling and color in the affected areas. It most often affects the nose, ears, cheeks, chin, fingers, or toes. Frostbite can permanently damage body tissues, and severe cases can lead to amputation. In extremely cold temperatures, the risk of frostbite is increased in patients with reduced blood circulation or not dressed properly.
Symptoms of frostbite include:
- Reduced blood flow to hands and feet (fingers or toes can freeze)
- Numbness
- Tingling or stinging
- Aching
- Bluish or pail, waxy skin
- Blanched (white) skin that does not return to normal after palpation
- If rewarmed, the patient could experience a numb or stinging sensation
- Firm or frozen feeling when palpated
- Parts of the skin may appear purple due to mottling in the affected area.
Frostbite management
In most cases, the patient with frostbite will be conscious and able to speak. The patient may or may not be experiencing hypothermia. As always, the primary survey will guide initial treatment. The following additional measures should be taken as soon as possible:
- Get into the warm ambulance as soon as possible.
- Handle gently
- Protect from further heat loss
- Do not allow the patient to exert them self
- Do not re-expose to the cold
- Remove any wet clothing and cover the patient with a blanket
- Do not break blisters or rub/massage affected areas
- Do not apply direct heat as the frostbite burns easily
- Do not rewarm if any chance of refreezing
- Do not give anything by mouth including warm liquids like coffee or tea.
Like a burn, the frostbitten extremity will swell which is why the medics should remove any jewelry. Handle the frostbitten extremity with care, including manual stabilization (an other rescuer will hold the frostbitten extremity to keep it from moving).
