Injuries To The Brain & Skull
Published (updated: ).
Everyone has bumped their head before. Often, the injury is minor because the skull is hard and it protects the brain. But other head injuries can be more severe, such as a skull fracture, concussion, or traumatic brain injury.
The most severe head injuries have no evidence of external trauma
Head injuries can be open or closed. A closed injury does not break through the skull. With an open, or penetrating, injury, an object pierces the skull and enters the brain. Closed injuries are not always less severe than open injuries making them difficult for medics to appreciate.
Brain injuries are less common than scalp injuries. Brain injuries can lead to a host of permanent injuries that may take years to recover, or worse, could lead to permanent neurological deficit. The degree of injury can be appreciated by EMS by the level of consciousness. Unresponsive patients will require the most amount of medical intervention. Head injury patients who are confused often are diagnosed with a cerebral concussion or mild diffuse axonal injury. In the past, concussions were seen as temporary problems that a patient could recover from; however, current thinking on this condition reveals that concussions likely result in permanent brain damage which can manifest as sleep loss, mood swings, and problems with memory). For this reason concussions are referred to as traumatic brain injures. Blunt force trauma can lead to bleeding around the brain which can lead to an immediate loss of consciousness (and quickly regaining consciousness) or neurological deficits as long as 24 hours after the injury occurred.
Scalp injuries often bleed more than expected due to the highly vascular nature of the scalp. Severe bleeding from the scalp can lead to shock in infants and young children.
Some common causes of head injuries are falls, motor vehicle accidents, violence, and sports injuries. It is important to know the warning signs of a moderate or severe head injury. Transport immediately if the injured person has:
- A headache that gets worse or does not go away
- Repeated vomiting or nausea
- Convulsions or seizures
- An inability to wake up
- Dilated (enlarged) pupil in one or both eyes
- Slurred speech
- Weakness or numbness in the arms or legs
- Loss of coordination
- Increased confusion, restlessness, or agitation
EMS management of head injuries

Initial management of the head injury patient should be guided by the primary survey. Noting the patient’s initial level of consciousness is critical in later diagnosis. Unconscious patients always require direct assessment of the airway. Airway is assessed by opening the airway, observing chest rise, and listening for adventitious (abnormal sounds like gurgling or stridor) sounds coming from the mouth.
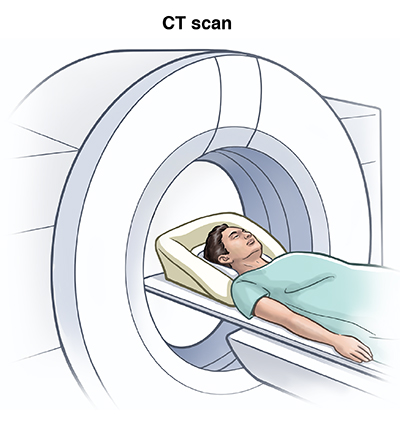
Since head injuries are sometimes much worse then they seem, transport to a facility where doctors can use a neurologic exams and imaging tests to make a diagnosis is necessary. The first clue for the ambulance crew is mechanism of injury. If a patient bumped their head on a doorway, the mechanism of injury would probably not lead the rescuers to think the injury is significant or is more than meets the eye. Conversely, if a patient falls off the roof and hits their head, the index of suspicion (idea of what is wrong) should lead EMS to consider the possibility of a more serious injury. The second clue is the patient’s level of consciousness and orientation. Patients who are confused or unconscious (either currently or after the injury) should be considered to have sustained a serious head injury and should be transported to a capable hospital. The medical community uses the Glasgow coma scale to determine a patient mental status:
The Glasgow Coma Scale (GCS) measures the following functions:
Eye Opening (E)
- 4 = spontaneous
- 3 = to sound
- 2 = to pressure
- 1 = none
Verbal Response (V)
- 5 = orientated
- 4 = confused
- 3 = words, but not coherent
- 2 = sounds, but no words
- 1 = none
Motor Response (M)
- 6 = obeys command
- 5 = localizing
- 4 = normal flexion
- 3 = abnormal flexion
- 2 = extension
- 1 = none
Clinicians use this scale to rate the best eye opening response, the best verbal response, and the best motor response an individual makes. The final GCS score or grade is the sum of these numbers.
Using the Glasgow Coma Scale
A patient’s Glasgow Coma Score (GCS) should be documented on a coma scale chart. This allows for improvement or deterioration in a patient’s condition to be quickly and clearly communicated.
Every brain injury is different, but generally, brain injury is classified as:
- Severe: GCS 8 or less
- Moderate: GCS 9-12
- Mild: GCS 13-15
Mild brain injuries can result in temporary or permanent neurological symptoms and neuroimaging tests such as CT scan or MRI may or may not show evidence of any damage.
Moderate and severe brain injuries often result in long-term impairments in cognition (thinking skills), physical skills, and/or emotional/behavioral functioning.
Obvious bleeding should be addressed with the application of direct pressure (pressure may need to be applied by a rescuer throughout transport).
