Personal Protective Equipment
Published (updated: ).
Standard precautions work under the assumption of that all patients have a contagious disease. There is no way to know if a patient has a contagious disease, therefore using standard precautions for all patients is a key skill to possess in the prehospital environment. Understanding the threat and possessing situational awareness will ensure the EMS crew will avoid contracting a contagious disease.
Contagious diseases are typically spread through the following routes:
- Airborne – A patient coughs or breaths and releases microscopic water particles infused with pathogens.
- Bloodborne – An infected sharp has penetrated the skin of a patient and then penetrates the skin of an EMS provider. Also, the EMS provider has been exposed to blood on non intact skin (a cut or lesion).
- Contact – Some microorganisms live in surfaces and can result in the EMS provider contracting a disease simply because they touched a contaminated object or patient.
- Vector borne – An insect or animal transmits a disease to an EMS provider. Malaria is an example of a vector borne disease.
- Food borne – Various types of bacteria and viruses live on the very food. Think twice before considering the merits of that next roller dog!
Good Hand Washing is the Best Way to Prevent The Spread of Disease
The most important measure to prevent the spread of infection is to wash your hands. Hand washing should be performed by rinsing your hands, lathering with soap for 15 seconds then drying your hands. Hand washing should always be performed prior to and after using the restroom, after each patient contact. When there are no facilities for hand washing, using a waterless hand gel is a reasonable substitute. Repeated hand washing and application of waterless hand sanitizer often results in dry hands making the application of skin moisturizer necessary.
If the rescuers hands have become contaminated with blood or body fluids then hand washing should become an immediate priority. Many rescuers worry about the possibility of contracting a disease when blood or body fluids have come in contact with their skin, however this concern is generally unfounded assuming the skin of the rescuer was intact (meaning there were no cuts or lesions on the skin). Gloves should be worn when there is a risk of exposure to blood or body fluids. Nitrile gloves are now common due to the confluence of latex allergies. Many EMS providers wear gloves all the time for every patient contact; however, wearing gloves will offer little or no protection against a contagious respiratory illness like meningitis or even COVID-19.
Eye protection is typically used to protect eyes from splash or spray of body fluids. Eyes are extremely vulnerable to infection, wearing goggles will minimize the risk. Eye protection should be worn at all times as rescuers often forget to put the goggles on. High risk procedures such as delivering a baby, managing profuse bleeding, or any airway management should be preceded by wearing eye protection despite the actual risk.
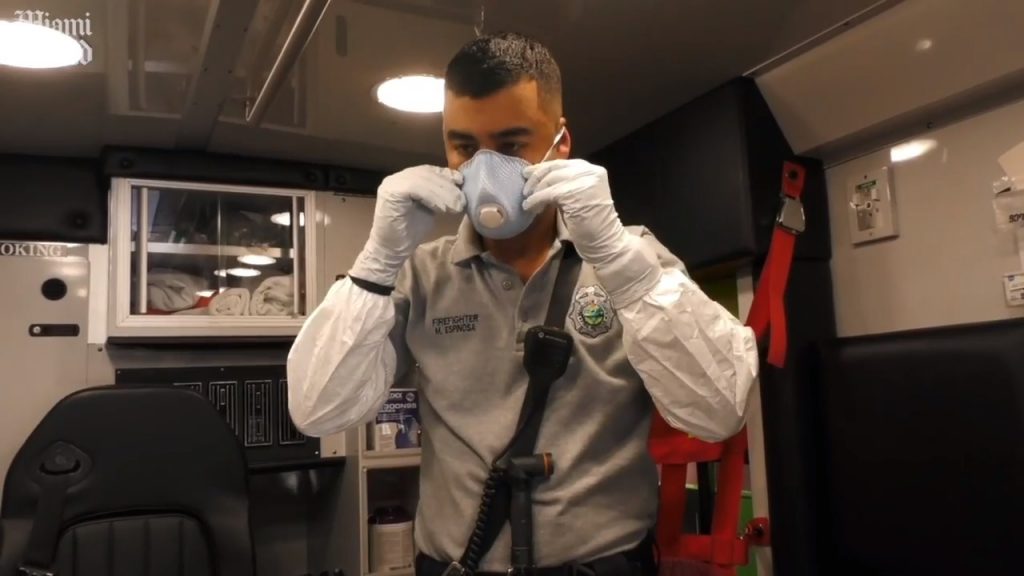
To protect the rescuer from contracting a respiratory illness, it is recommended that EMS providers wear N-95 masks. An N-95 mask filters out 95% of all particulates (there are even N-100 masks as well). Wearing a mask is unpleasant and even socially awkward. Surgical masks can be worn by the patient to prevent spreading the illness to EMS or other medical personnel. Many patients will be unable to tolerate a surgical mask. A non-rebreather mask with oxygen can provide some limited barrier between the EMS crew and the patient.
Without exception, sharps should be discarded into a sharps container. Sharps containers should be changed out before they are full. Employers have very specific procedures for processing medical waste.

