Defibrillation
Published .
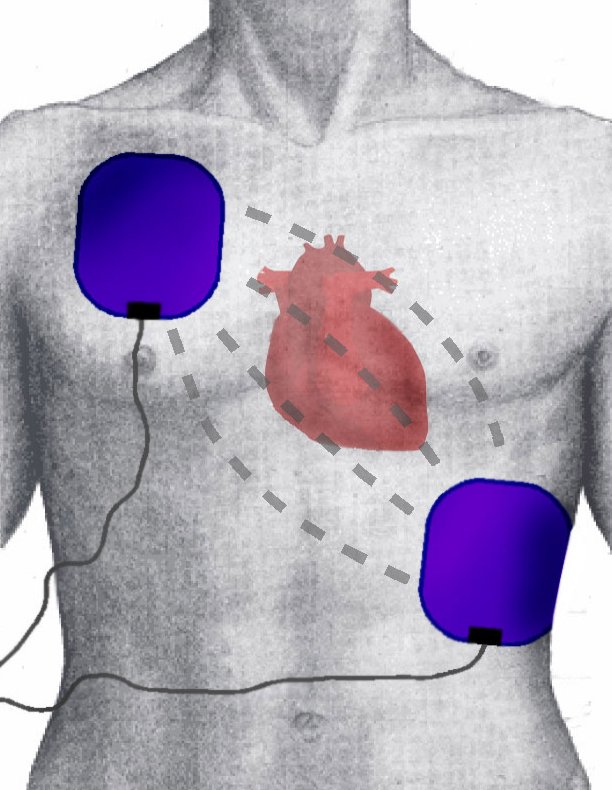
Cardiac defibrillation is the act of administering a transthoracic electrical current to a person experiencing one of the two lethal ventricular dysrhythmias, ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). Under Advanced Cardiac Life Support (ACLS) guidelines, pulseless VT and VF are treated the same. Heart disease remains the number one cause of death in both sexes. About half of these sudden deaths occur in the pre-hospital setting; of these, almost three-quarters happen in the home, and half of these are unwitnessed. In the adult patient, VF is the most common cause of sudden cardiac arrest. The definitive treatment for VF is to perform electrical defibrillation. When defibrillation is delayed, effectiveness is reduced by almost 10% per minute.
Cardiac defibrillation is the act of administering a transthoracic electrical current to a person experiencing one of the two lethal ventricular dysrhythmias, ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). Under Advanced Cardiac Life Support (ACLS) guidelines, pulseless VT and VF are treated the same.
According to the Centers for Disease Control and Prevention (CDC), 610,000 deaths occur annually in the United States from heart disease. Heart disease remains the number one cause of death in both sexes. About half of these sudden deaths occur in the pre-hospital setting; of these, almost three-quarters happen in the home, and half of these are unwitnessed. In the adult patient, VF is the most common cause of sudden cardiac arrest.
The definitive treatment for VF is to perform electrical defibrillation. Defibrillation is highly effective in terminating VF when performed as close to the onset of VF as possible. When defibrillation is delayed, effectiveness is reduced by almost 10% per minute.
Adult victims of nontraumatic cardiac arrest who receive resuscitation attempts by emergency medical services have a rate of survival to hospital discharge of only 10.8%. In comparison, adult patients who develop cardiac arrest in a hospital have rates of survival to hospital discharge of up to 25.5%. This increased survival is due to defibrillation being performed closer to the onset of VF.

Ventricular fibrillation occurs when the normal transmission of the cardiac impulse through the heart’s electrical conduction system is interrupted. This can occur in the setting of coronary ischemia or acute myocardial infarction. It can also occur due to sudden interruptions to the cardiac impulse by events such as an electrical shock; a blow to the chest (commotio cordis); premature ventricular contractions, especially the “R on T” type; abnormal tachycardic rhythms such as ventricular tachycardia; and syndromes such as QT prolongation.
The chaotic, dysrhythmic firing of multiple irritable myocardial foci in the ventricles causes fibrillation of the ventricles. This produces a loss of normal ventricular contraction with the resultant cessation of cardiac output. The clinical result is a sudden cardiac arrest. While defibrillation is highly effective in treating VF and pulseless VT, its effectiveness is time-dependent. Untreated VF will rapidly deteriorate into asystole, from which resuscitation rates are dismal. For untreated VF or VT, the likelihood of resuscitation decreases by up to 10% per minute. Cardiopulmonary Resuscitation (CPR) can provide temporary oxygenation and circulation until defibrillation becomes available. Conventional manual CPR, combining chest compressions with rescue breathing, when done properly, can provide up to 33% of normal cardiac output and oxygenation. The provision of early CPR can triple the rate of survival from witnessed sudden cardiac arrest.
The definitive treatment for VF or its equivalent, pulseless VT, is electrical defibrillation. Defibrillation, contrary to popular belief, does not “jump-start” the heart. Rather, it produces nearly simultaneous depolarization of a critical mass of myocardium, causing momentary cessation of all cardiac activity. Under ideal circumstances, a viable site within the heart’s intrinsic electrical conduction system will then spontaneously initiate an electrical impulse that can restore normal propagation of the heart’s cardiac cycle, with a resultant restoration of ventricular contraction and, hence, a pulse. Traditional “manual” defibrillation is provided by medical or paramedical personnel trained in electrocardiogram (EKG) dysrhythmia recognition and emergency cardiac care. Today, the widespread availability of automated external defibrillators (AEDs) allows trained first responders and, in some instances, the lay public to provide early defibrillation to victims of sudden cardiac arrest. AEDs interpret the EKG rhythm automatically, determine if a “shockable” rhythm is present, self-charge to the required energy level, and provide the responder with verbal prompts to successfully perform the defibrillation process
