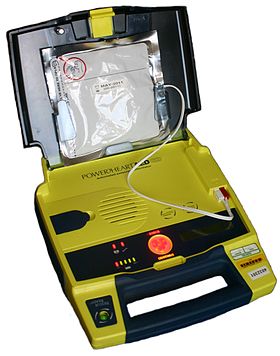
Automated External Defibrillator
Published (updated: ).
An automated external defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm.
With simple audio and visual commands, AEDs are designed to be simple to use for the layperson, and the use of AEDs is taught in many first aid, certified first responder, and basic life support (BLS) level cardiopulmonary resuscitation (CPR) classes.
Conditions that the device treats
An automated external defibrillator is used in cases of life-threatening cardiac arrhythmias which lead to sudden cardiac arrest, which is not the same as a heart attack. The rhythms that the device will treat are usually limited to:
- Pulseless Ventricular tachycardia (shortened to VT or V-Tach)
- Ventricular fibrillation (shortened to VF or V-Fib)
In each of these two types of shockable cardiac arrhythmia, the heart is electrically active, but in a dysfunctional pattern that does not allow it to pump and circulate blood. In ventricular tachycardia, the heart beats too fast to effectively pump blood. Ultimately, ventricular tachycardia leads to ventricular fibrillation. In ventricular fibrillation, the electrical activity of the heart becomes chaotic, preventing the ventricle from effectively pumping blood. The fibrillation in the heart decreases over time, and will eventually reach asystole.
AEDs, like all defibrillators, are not designed to shock asystole (‘flat line’ patterns) as this will not have a positive clinical outcome. The asystolic patient only has a chance of survival if, through a combination of CPR and cardiac stimulant drugs, one of the shockable rhythms can be established, which makes it imperative for CPR to be carried out prior to the arrival of a defibrillator.
Uncorrected, these cardiac conditions (ventricular tachycardia, ventricular fibrillation, asystole) rapidly lead to irreversible brain damage and death, once cardiac arrest takes place. After approximately three to five minutes in cardiac arrest, irreversible brain/tissue damage may begin to occur. For every minute that a person in cardiac arrest goes without being successfully treated (by defibrillation), the chance of survival decreases by 7 percent per minute in the first 3 minutes, and decreases by 10 percent per minute as time advances beyond ~3 minutes.
Preparation for operation
Most manufacturers recommend checking the AED before every period of duty or on a regular basis for fixed units. Some units need to be switched on in order to perform a self check; other models have a self check system built in with a visible indicator.
All manufacturers mark their electrode pads with an expiration date, and it is important to ensure that the pads are in date. The typical life expectancy of AED pads are between 18 and 30 months. This is usually marked on the outside of the pads. Some models are designed to make this date visible through a ‘window’, although others will require the opening of the case to find the date stamp.
It is also important to ensure that the AED unit’s batteries have not expired. The AED manufacturer will specify how often the batteries should be replaced. Each AED has a different recommended maintenance schedule outlined in the user manual. Common checkpoints on every checklist, however, also include a monthly check of the battery power by checking the green indicator light when powered on, condition and cleanliness of all cables and the unit, and check for the adequate supplies.
Mechanism of operation
An AED is “automatic” because of the unit’s ability to autonomously analyze the patient’s condition. To assist this, the vast majority of units have spoken prompts, and some may also have visual displays to instruct the user.
“External” refers to the fact that the operator applies the electrode pads to the bare chest of the victim (as opposed to internal defibrillators, which have electrodes surgically implanted inside the body of a patient).
When turned on or opened, the AED will instruct the user to connect the electrodes (pads) to the patient. Once the pads are attached, everyone should avoid touching the patient so as to avoid false readings by the unit. The pads allow the AED to examine the electrical output from the heart and determine if the patient is in a shockable rhythm (either ventricular fibrillation or ventricular tachycardia). If the device determines that a shock is warranted, it will use the battery to charge its internal capacitor in preparation to deliver the shock. The device system is not only safer – charging only when required, but also allows for a faster delivery of the electric current.
When charged, the device instructs the user to ensure no one is touching the patient and then to press a button to deliver the shock; human intervention is usually required to deliver the shock to the patient in order to avoid the possibility of accidental injury to another person (which can result from a responder or bystander touching the patient at the time of the shock). Depending on the manufacturer and particular model, after the shock is delivered most devices will analyze the patient and either instruct CPR to be performed, or prepare to administer another shock.
Many AED units have an ‘event memory’ which store the ECG of the patient along with details of the time the unit was activated and the number and strength of any shocks delivered. Some units also have voice recording abilities to monitor the actions taken by the personnel in order to ascertain if these had any impact on the survival outcome. All this recorded data can be either downloaded to a computer or printed out so that the providing organization or responsible body is able to see the effectiveness of both CPR and defibrillation. Some AED units even provide feedback on the quality of the compressions provided by the rescuer.
