Hemodialysis
Published (updated: ).
Renal Failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys are functioning at less than 15% of normal levels. Kidney failure is classified as either acute kidney failure, which develops rapidly and may resolve; and chronic kidney failure, which develops slowly and can often be irreversible. Symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications of acute and chronic failure include uremia, high blood potassium, and volume overload. Complications of chronic failure also include heart disease, high blood pressure, and anemia.
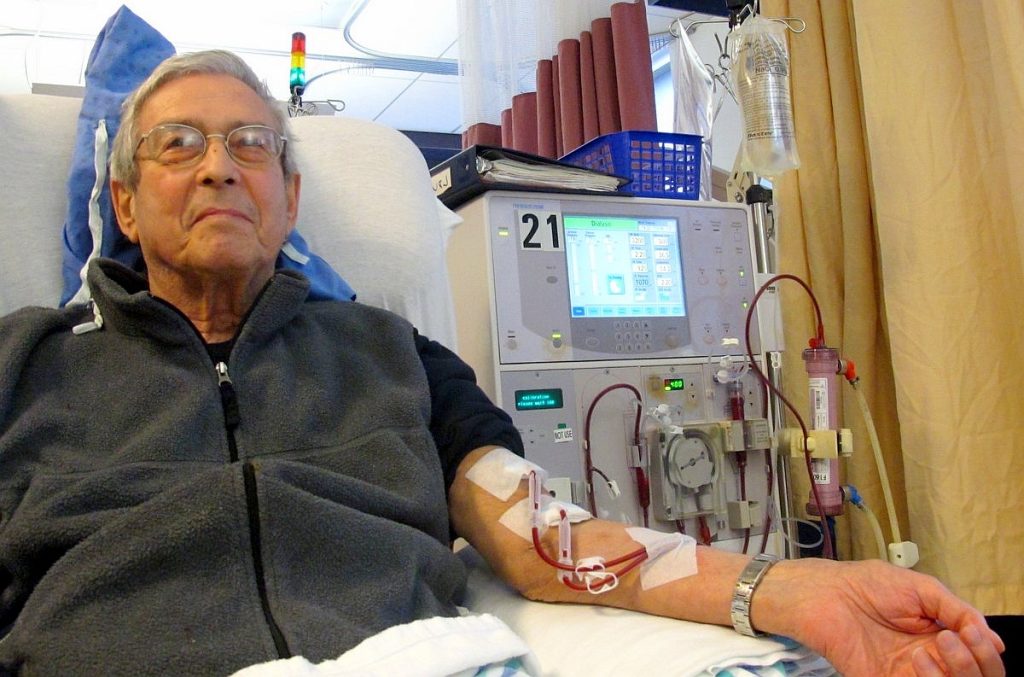
Hemodialysis is a treatment to filter wastes and water from blood, as the patient’s kidneys did when they were healthy. Hemodialysis helps control blood pressure and balance important minerals, such as potassium, sodium, and calcium, in the blood. Hemodialysis can help the patient feel better and live longer, but it’s not a cure for kidney failure.
What happens during hemodialysis?
During hemodialysis, the blood goes through a filter, called a dialyzer, outside the body. A dialyzer is sometimes called an “artificial kidney.”
At the start of a hemodialysis treatment, a dialysis nurse or technician places two needles into the arm. . Each needle is attached to a soft tube connected to the dialysis machine.

The dialysis machine pumps blood through the filter and returns the blood to the body. During the process, the dialysis machine checks the blood pressure and controls how quickly
- Blood flows through the filter
- Fluid is removed from the body
Common problems associated with dialysis patients

Dialysis is a grueling procedure for the patient. The patient’s blood is pumped out of their body and ran through a machine. The result is often hypotension. Hypotension results from the dialysis clinic removing too much fluid out of the patient’s blood, leaving the patient with less circulating blood volume. Clinicians should not obtain a blood pressure in the arm with the dialysis shunt or fistula. Dialysis shunts or fistulas are surgically implanted into the patient and enables the dialysis clinic to gain vascular access more quickly. Sometimes the fistula or dialysis shunt is bleeding profusely. Very often, the patient complains of nausea and shortness of breath. The shortness of breath is more common prior to dialysis and is the result of the patient being fluid overloaded (especially if they missed an appointment). Dialysis patients also experience frequent infections to their dialysis access site.
Peritoneal Dialysis
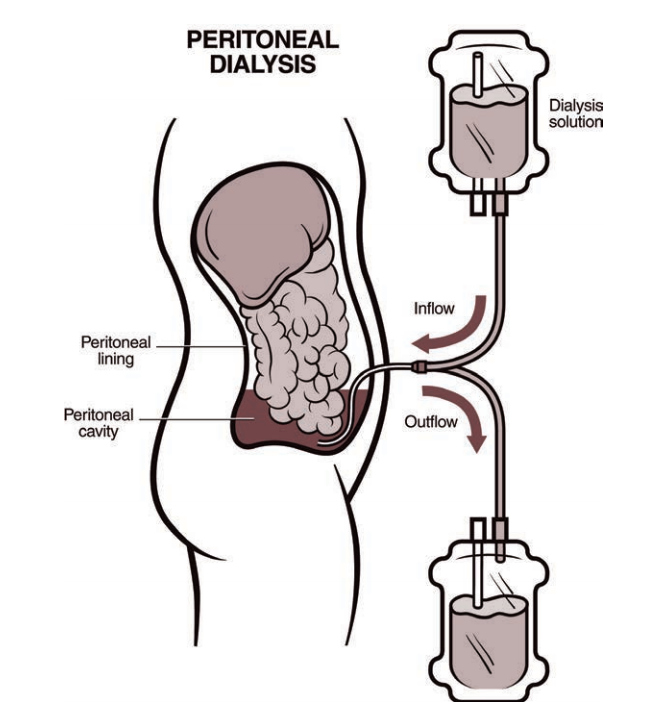
Peritoneal dialysis removes waste and extra fluid through the blood vessels that line the walls of the abdomen. A membrane called the peritoneum covers the walls of the abdomen. Peritoneal dialysis involves putting a soft, hollow tube (catheter) into the abdominal cavity and filling it with a cleansing fluid (dialysis solution). The solution contains a type of sugar that draws out waste and extra fluid. The waste and fluid passes from the blood vessels through the peritoneum and into the solution. After a set amount of time, the solution and waste is drained and thrown away.
The process of filling and draining the abdomen is called an exchange. The length of time the cleansing fluid remains in the body is called the dwell time. The number of exchanges and amount of dwell time depends on the method of peritoneal dialysis used and other factors. A physician will perform surgery to place a catheter in the abdomen where it will stay. It is most often near the belly button.
Assessment and management of dialysis patients
Ambulance crews are often used to transport dialysis patients to and from dialysis. The dialysis center should not release patients with out of control bleeding and hypotension, but sometimes they do. Before the patient is moved to the ambulance, the medics need to assess the dialysis shunt to ensure it is not bleeding and check the patient’s blood pressure. It may be necessary to delay departure from the dialysis clinic to the patient’s home in order to allow the blood pressure to normalize. If the dialysis shunt is bleeding, it may be necessary to transport the patient to the ER while applying direct pressure to stop the bleeding. If the patient is hypotensive, positioning the patient with their feet elevated can increase blood pressure. Obviously, patients with shortness of breath need oxygen and will not tolerate being positioned with their feet elevated. If the patient is experiencing shortness of breath after dialysis, transport to the ER may be a better option than to the patient’s home.
