Respiratory Distress
Published .
The primary survey
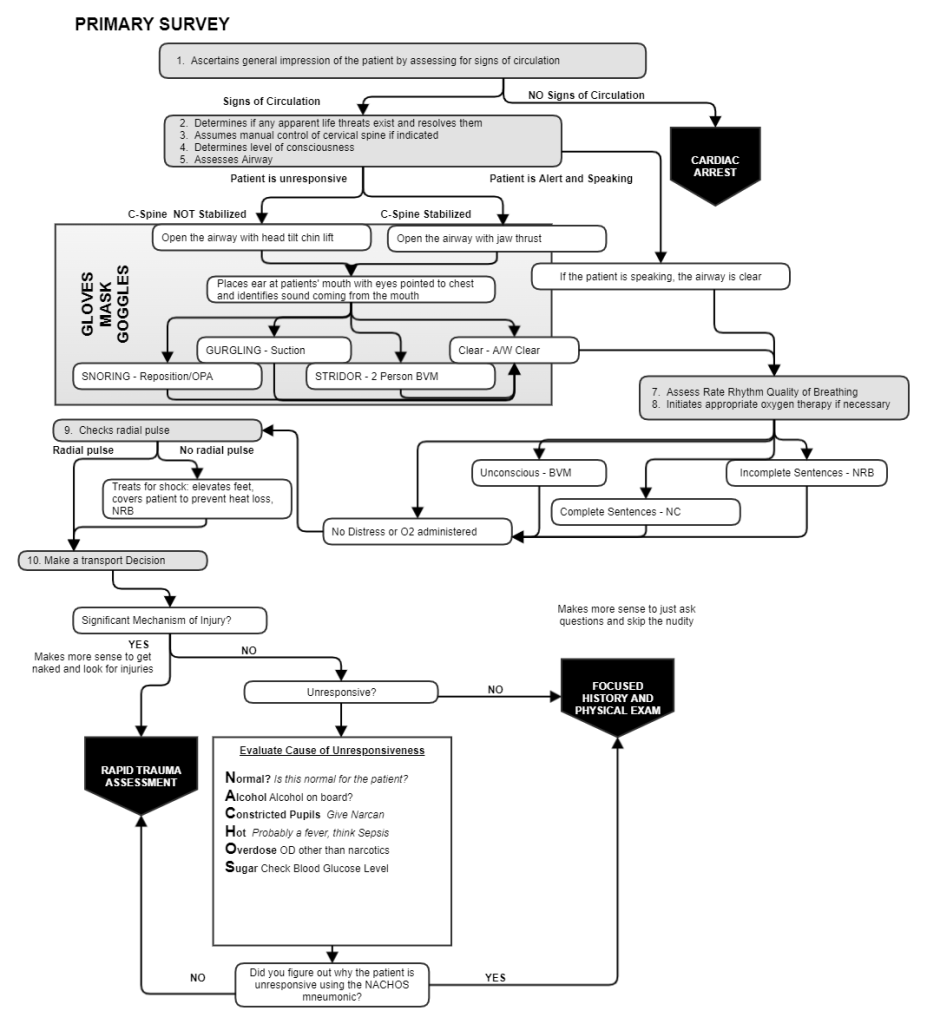
The primary assessment begins when the ambulance crew makes contact with the patient and answers numerous questions about how the rest of the call will be conducted. Will the patient need CPR? Is the patient unresponsive? Does the patient need oxygen or ventilation?
Patients generally don’t need ventilation if they are alert and talking with EMS, but the patient can still have shortness of breath. If left untreated, the patient’s respiratory distress could become worse right before the eyes of the ambulance crew. Administering supplemental oxygen via non rebreather mask can delay the patient’s downward spiral into respiratory arrest. When evaluating the patient’s breathing during the primary survey, minimally count the rate, rhythm, and quality of breathing. Some other clues that the patient is experiencing shortness of breath are:
- Restlessness
- Increased heart rate
- Changes in respiratory rate or rhythm
- Skin color changes
- Abnormal sounds of breathing (like wheezing or stridor)
- Inability to speak in complete sentences
- Accessory muscle usage
- Altered mental status
- Abdominal breathing
- Coughing
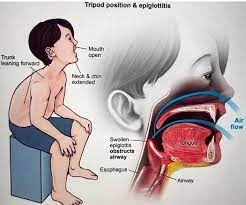
- Tripod position
For the conscious patient, initial management is easy; just give 15 liters per minute via non rebreather mask. Positioning the patient in a sitting position (fowlers or semi-fowlers position) will help, but usually the conscious patient is already sitting upright when the ambulance arrives.
