EMS Treatment of Stroke
Published .
EMS role in stroke is early indentification
The ambulance crew has got be on the lookout for stroke. Stroke should be strongly considered when the patient has a neurological deficit of any kind and a normal or high blood glucose level. The number one mimic of stroke is hypoglycemia; ruling out hypoglycemia is easy to do with a glucometer. The goal is find the patient and get them to the hospital within 3 hour from the onset of symptoms. What that means for the ambulance crew is they almost have to walk out with the patient as soon as they get to the patient’s house in order to make this 3 hour window of treatment work.
The hospital won’t treat the patient without knowing the patients medications, history, and drug allergies. By having all of this information ready for the hospital, the ambulance crew will save valuable minutes while the patient is being considered for risky thrombolytic therapy. Thrombolytics are a classification of drug that breaks up blood clots. The idea is that the thrombolytics will open up the blood vessels in the brain, restore circulation before any permanent disability is possible.
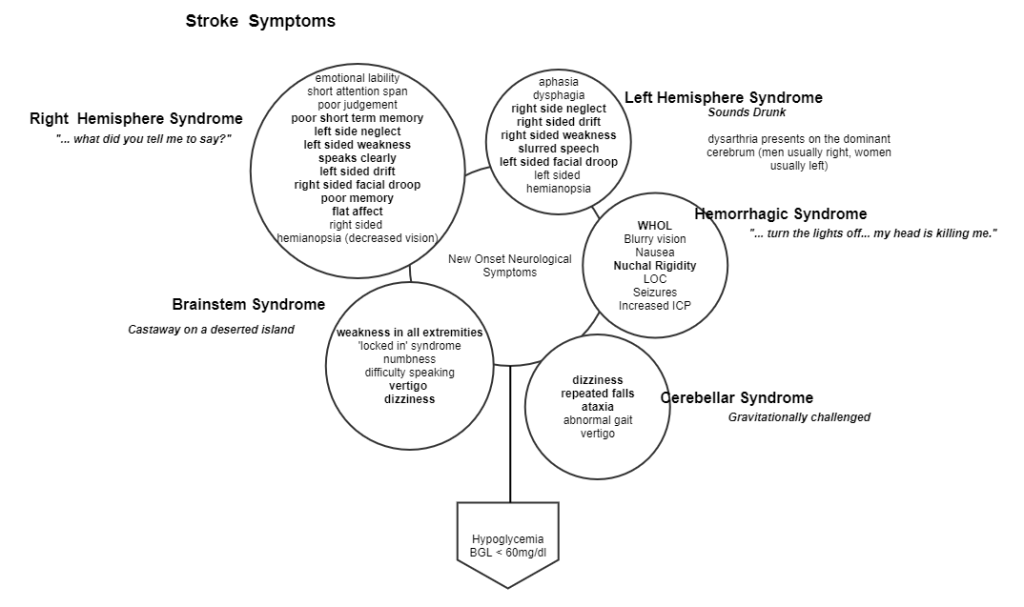
How a stroke can give different symptoms
Different parts of the brain have different functions. For instance in most people, the right hemisphere of the brain deals with speech. A stroke to the right hemisphere of the brain often results in dysphasia (difficulty speaking). A stroke in the brainstem results in the patient seemingly having a stroke in their entire body. Patient’s with a hemorrhagic stroke will often have a severe headache.
The Cincinnati Prehospital Stroke Scale
- Facial droop: Have the person smile or show his or her teeth. If one side doesn’t move as well as the other so it seems to droop, that could be a sign of a stroke.
- Normal: Both sides of face move equally
- Abnormal: One side of face does not move as well as the other (or at all)
- Arm drift: Have the person close his or her eyes and hold his or her arms straight out in front with palms facing up for about 10 seconds. If one arm does not move, or one arm winds up drifting down more than the other, that could be a sign of a stroke.
- Normal: Both arms move equally or not at all
- Abnormal: One arm does not move, or one arm drifts down compared with the other side
- Speech: Have the person say, “You can’t teach an old dog new tricks,” or some other simple, familiar saying. If the person slurs the words, gets some words wrong, or is unable to speak, that could be a sign of a stroke.
- Normal: Patient uses correct words with no slurring
- Abnormal: Slurred or inappropriate words or mute
Patients with 1 of these 3 findings as a new event have a 72% probability of an ischemic stroke. If all 3 findings are present the probability of an acute stroke is more than 85%
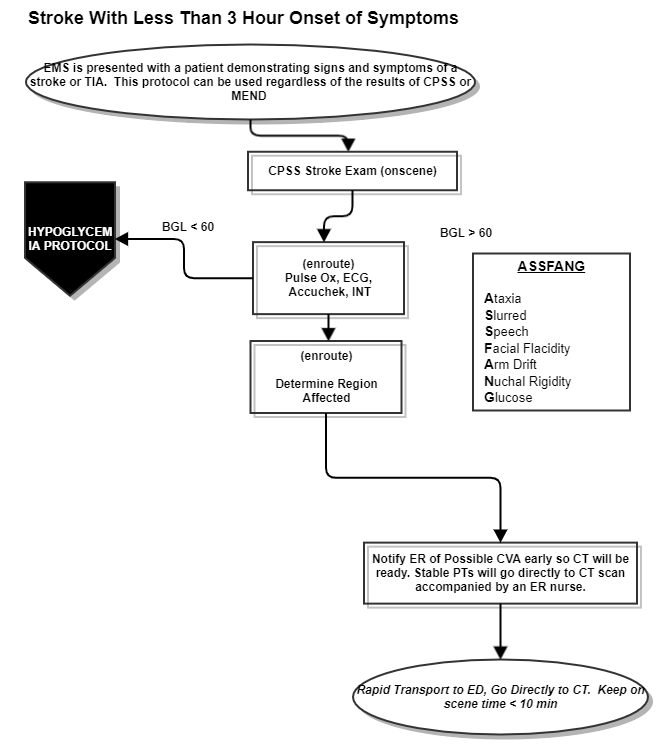
Treatment
Oxygen is not indicated unless the patient is also experiencing shortness of breath or has a low pulse oxygen saturation level. Rapid transport and communication with the ER is critical. Stroke patients need to be transported to a stroke center. At most stroke centers, the ambulance crew will be met in the ER by the nurse and led to the Computerized Tomography (CT) scanner. Once the scan is complete, the ambulance crew will usually bring the patient to the ER and give a report to the nurse. Of critical importance to the patient is name, DOB, medical history, medications, drug allergies, and time of onset. Without being able to solidly establish the time of onset of symptoms, the risk of giving thrombolytics suddenly becomes greater than the benefit.
