Seizures
Published (updated: ).
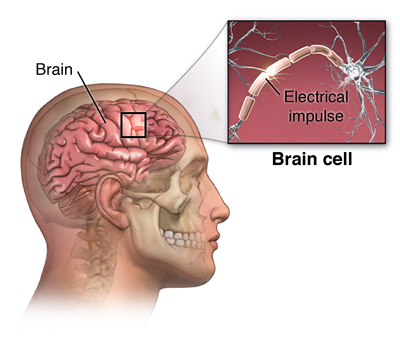
Epilepsy is a disorder of the brain. People are diagnosed with epilepsy when they have had two or more seizures. There are many types of seizures. A person with epilepsy can have more than one type of seizure.
The signs of a seizure depend on the type of seizure.
Sometimes it is hard to tell when a person is having a seizure. A person having a seizure may seem confused or look like they are staring at something that isn’t there. Other seizures can cause a person to fall, shake, and become unaware of what’s going on around them. Learn about different types of seizures and their signs and symptoms so you can tell when someone is having a seizure.
Seizures are classified into two groups.
- Generalized seizures affect both sides of the brain.
- Absence seizures, sometimes called petit mal seizures, can cause rapid blinking or a few seconds of staring into space.
- Tonic-clonic seizures, also called grand mal seizures, can make a person
- Cry out.
- Lose consciousness.
- Fall to the ground.
- Have muscle jerks or spasms.
The person may feel tired after a tonic-clonic seizure.
- Focal seizures are located in just one area of the brain. These seizures are also called partial seizures.
- Simple focal seizures affect a small part of the brain. These seizures can cause twitching or a change in sensation, such as a strange taste or smell.
- Complex focal seizures can make a person with epilepsy confused or dazed. The person will be unable to respond to questions or direction for up to a few minutes.
- Secondary generalized seizures begin in one part of the brain, but then spread to both sides of the brain. In other words, the person first has a focal seizure, followed by a generalized seizure.
Seizures may last as long as a few minutes but usually only last for around 30 seconds. When the EMS crew is describing a seizure, they are typically describing a generalized tonic clonic seizure that is usually accompanied by the following symptoms:
- Spasms, muscle contractions
- Bitten tongue, increased secretions
- Sweating
- Cyanosis
- Unconscious with gradually increasing level of consciousness
- Incontinent
- Amnesia of the event.
The postictal phase
The postictal state is a period that begins when a seizure subsides and ends when the patient returns to baseline. It typically lasts between 5 and 30 minutes and is characterized by disorienting symptoms such as confusion, drowsiness, hypertension, headache, nausea, etc.
The postictal state is an abnormal condition that lasts for a period that begins when a seizure subsides and ends when the patient returns to baseline. Marking the termination of a seizure and the return to baseline is straightforward only in a limited number of cases. The difficulty of distinguishing ictal from the postictal period may depend on the type of seizure. It is easier to determine the end of the seizure and the beginning of the postictal state for a generalized tonic-clonic or a generalized tonic seizure.
Administering oxygen seems to help decrease the time the patient is in the post ictal phase.
Status Seizures
A status seizure is a seizure that lasts longer than a couple of minutes or has seizures despite being in the postictal phase. Status seizures are dangerous and are really the major focus of EMS treatment of seizures. Most seizure calls are not really life threatening. A status seizure can kill an adult in as little as 10 minutes. While the seizure activity is raging, the patient’s respiratory drive is inhibited. Status seizure patients often die of hypoxia. Some patient even stop breathing while they are seizing.
First time seizures are also serious
Most of the time, seizure patients have a history of seizures and either experience a breakthrough seizure (the medications don’t totally stop the seizures) or stop taking their medication and have another seizure (medication noncompliance). What about patient’s who are having a seizure for the first time? The cause of the seizure is yet to be determined and the trail grows colder by the second. It’s time for EMS to round up the usual suspects:
Nearly every cause of altered mental status has a definitive test. When the ambulance crew assesses a patient with altered mental status, they will not have the advantage of a myriad of clinical tests. What the ambulance crew needs is an easy way to assess common causes of altered mental status. When the patient is conscious, the ambulance crew should use the SPASTIC pneumonic:
Sugar – Check patients blood glucose level
Poisons/Pregnancy – Inquire about the possibility of poisoning. A condition associated with pregnancy called eclampsia can cause seizures.
Alcohol – Do the rescuers smell alcohol?
Trauma – Is there a history of a head injury?
Stroke – Could the patient be having a stroke
Infection – Is the patient running a fever?
Crack or other drugs – Is the patient on drugs?
