What To Do When The Patient Is Unconscious And There Is No MOI
Published (updated: ).
When the patient is unconscious, they are not in a position to tell you what’s wrong
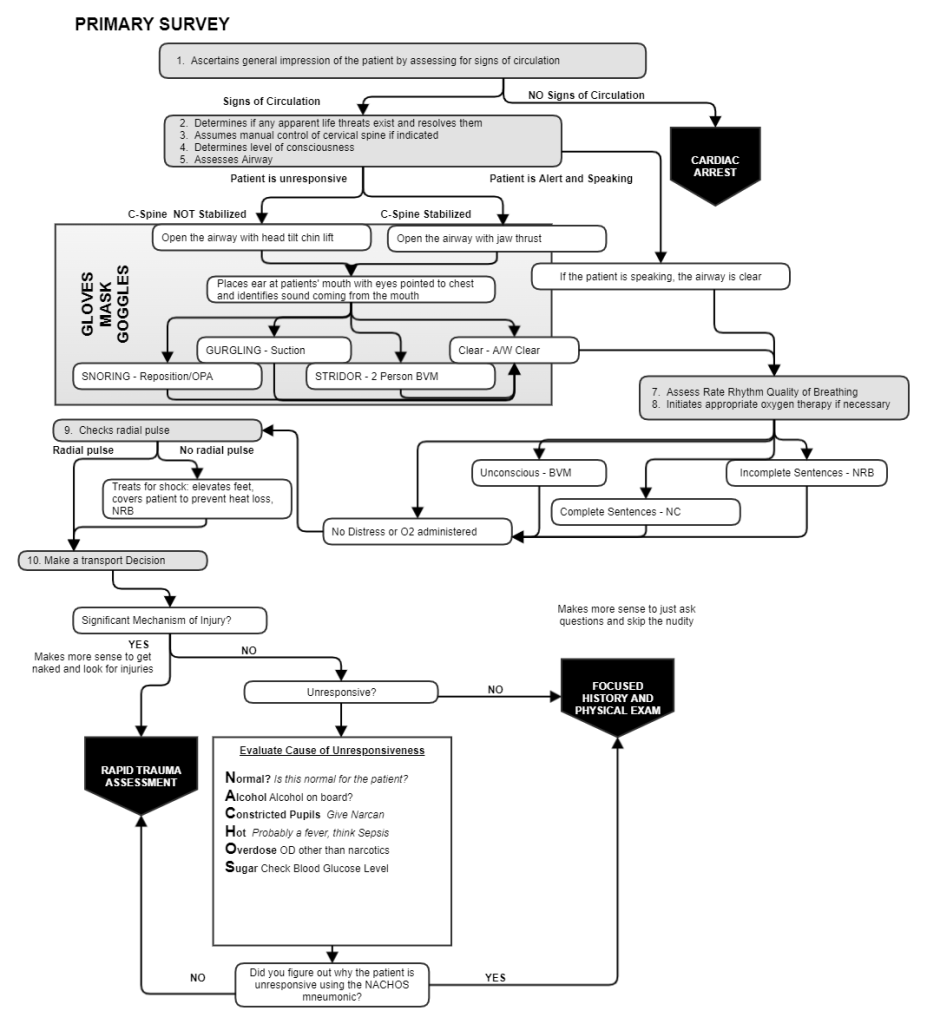
If the patient had fallen off the roof of their house and was found unconscious, the medics should be thinking head injury or spinal cord injury. If the patient had been hit by a car and was unconscious, the medics should be thinking the patient hit their head or has a spinal cord injury. If unconscious patient had been shot and was found in a pool of blood the medics should be thinking about hypovolemic shock. These findings would lead the EMS crew to start the rapid trauma assessment (assessment where the patient’s clothing is removed and the medics look for injuries).
But if there were no mechanism of injury? What if the patient was just found unresponsive? Should you still look for trauma?
The short answer is yes. Just as EMS should always be looking for a MOI despite being dispatched to a patient with chest pain. When a patient is unconscious, trauma must always be considered.
Would it change anything for the medics if they just knew why the patient was unconscious in the first place? If the medics knew that the patient was unresponsive because the patients blood sugar was too low, should they feel the need to cut off clothing? The answer is no. So what the medics need is a quick way to rule out some obvious causes of altered mental status. For this, georgiaemsacademy developed the NACHOS pneumonic.
- Normal – Is this normal for the patient. Sometimes patients you pick up are always unresponsive due to their condition. Maybe this is normal after the patient has a seizure. Maybe this is something that happens to the patient, and a third party called 911.
- Alcohol – Alcohol can cause altered mental status. It’s easy to tell if a person has been drinking just by smelling their breath
- Constricted Pupils – Constricted pupils tell the EMS crew that the patient has overdosed on a narcotic. Narcotics are central nervous system depressants that can stop patients from breathing.
- Hot – Patients that have a fever probably have an infection. An infection can lead to sepsis which can lead to septic shock. Hot skin could therefore explain why the patient is unresponsive.
- Otherwise overdose – A patient could have overdosed on a benzodiazepine or other drug that could explain the patients altered mental status.
- Sugar – Check the patient’s blood glucose level. If the blood glucose is under 60 mg/dl, the patient is experiencing hypoglycemia. If the patient is unresponsive, oral glucose can’t be given. Only AEMT’s and Paramedics can administer intravenous dextrose to raise the patient blood sugar level.
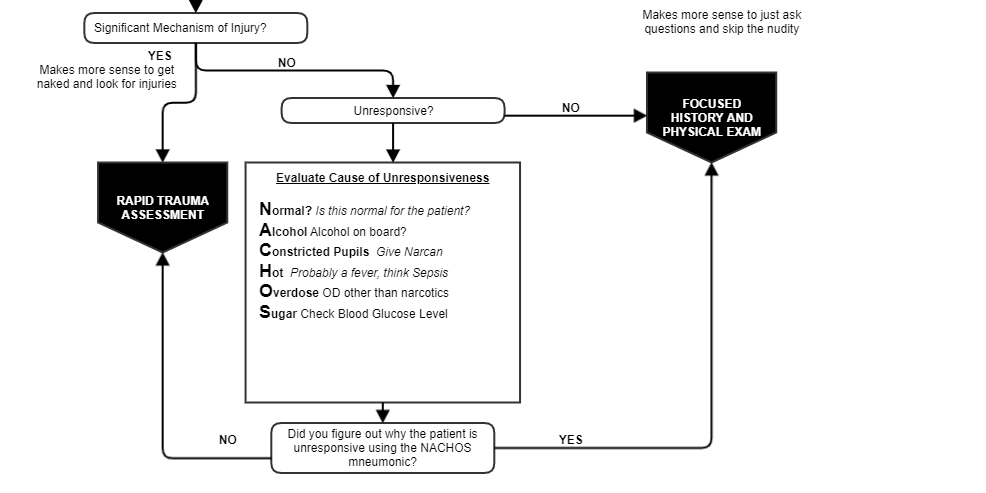
If the nature of unresponsiveness can be determined with NACHOS, the ambulance crew can just transport the patient to the hospital without worrying if they should be checking for injuries. Else, if the cause of the unresponsiveness can’t be found with NACHOS, the medics should immediately stabilize the cervical spine in the neutral and in line position and begin cutting the patient’s clothing to look for injuries.
