Meet The Patient With The Primary Survey
Published .

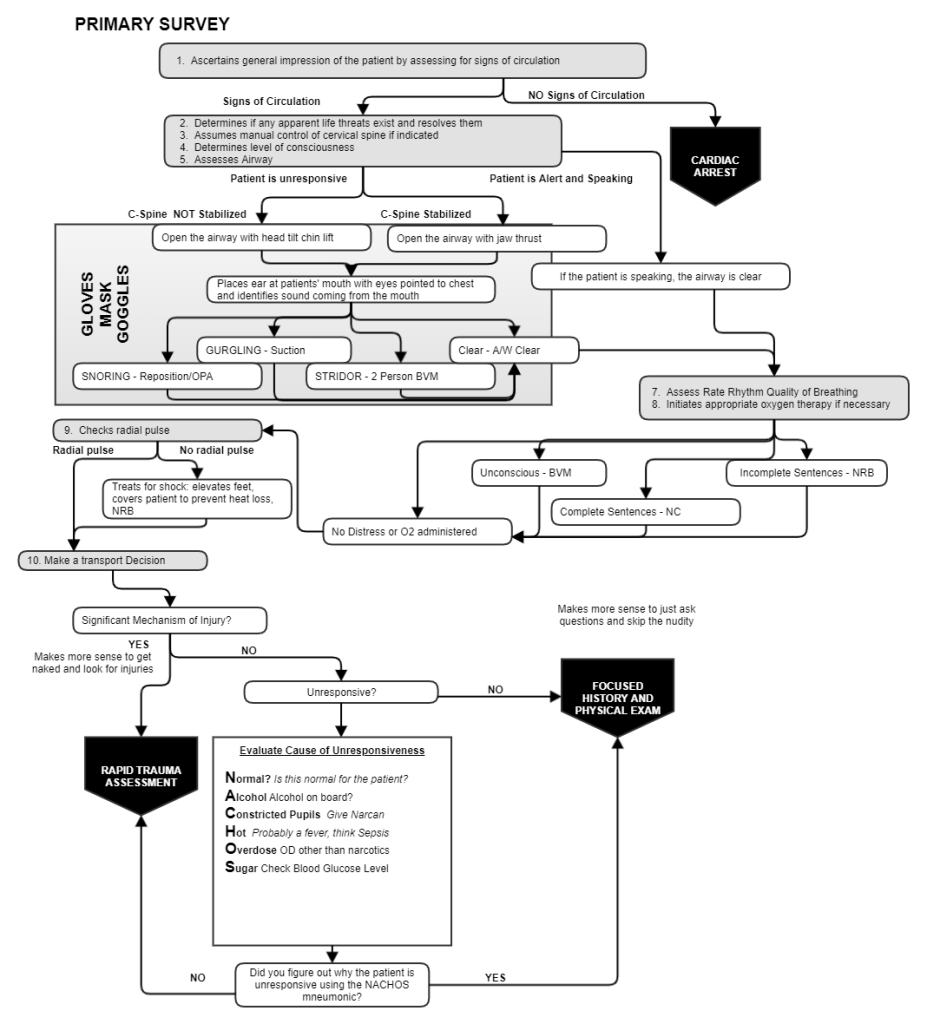
The primary survey identifies and treats patients who are in immediate need of resuscitation
The primary survey is how EMS meets every patient. The objective is to identify and treat patients needing resuscitation. Resuscitation is the action or process of reviving someone from unconsciousness or apparent death. There is nothing academic about the primary survey. The medic sees something and immediately does something about it. For this reason, the most important and finely polished skill taught at georgiaemsacademy.com is the primary survey. Georgiaemsacademy.com students would be wise to take listen to every word in these passages about primary survey. A primary survey can lead to numerous interventions:
- CPR
- Suctioning an airway
- Opening an airway
- Ventilating a patient
- Administering oxygen
- Treating for shock
- Stopping life threatening bleeding
Assess for signs of circulation
The first priority for the ambulance crew is to determine whether the patient possesses signs of circulation. Signs of circulation is any movement that would indicate the patient is alive. Even unconscious patients move when the breathe, but a patient in cardiac arrest is as motionless as a stone. If the patient does not exhibit signs of circulation, then the patient needs CPR. First ask the patient, “Do you need CPR?” If the patient does not answer, then the rescuers should find their hand placement and begin performing chest compressions.
Identify and treat apparent life threats

An apparent life threat is more of a threat than an injury. There are life threating injuries, but the apparent life threat is obvious, and must be resolved immediately. Very few things would qualify as an immediate life threat, examples are:
- Patient is on fire
- Patient is spurting blood
- Patient is actively being strangled
Manually stabilize the cervical spine (if indicated)

The only part of the scene size up that has any relevance to the primary survey is the determination that a mechanism of injury exists (MOI). The presence of an MOI tells the EMS crew that the possibility of a cervical spine fracture exists. The cervical spine is the portion of the spinal column that connects the head to the rest of the body. As such, this extremely vulnerable part of the spinal cord is subject to constant scrutiny by EMS and ER personnel alike. A spinal cord injury could result in the patient being paralyzed from the neck down for the rest of their life or could even cause the patient to stop breathing. Care in how the patient is moved, including how the airway is opened is determined from this observation. Regardless of the patient’s level of consciousness or airway, the patient’s cervical spine must be maintained in neutral (meaning the neck is neither flexed nor extended and inline position (meaning the nose is in line with the naval). If the head is flexed, extended, or not in line with the naval, the medics must move the neck to the neutral and in line position and maintain this position with manual stabilization.
Determine patient’s level of consciousness
Patients who are alert are talking, which tells the rescuers that the airway is clear. If the patient is not alert (verbally responsive, responsive to painful stimuli, or unresponsive) then the airway must be assessed to determine if it is clear. Determining the patient’s level of conscious is a critical step in determining if the airway is clear. How weird would it be for the patient to be talking to an ambulance crew, and the medics look at the patient’s mouth to see if there are any obstructions. Assessing the level of consciousness is a critical step in determining the if the airway is clear (patency).
Assess airway
If the patient is alert and talking to EMS, the airway is clear (at least for now). The matter of the airway becomes more complicated when the patient is not alert. In the case of a patient who is not alert, the airway must be opened, then the rescuers look, listen, and feel the breaths coming out of the patient’s mouth to determine if the airway is clear. If the MOI suggested a cervical spine fracture is possible, the EMS crew will open the airway with the jaw thrust technique. If the rescuers are not concerned about the condition of the cervical spine (because there is no MOI), then the rescuers will open the airway with the head tilt chin lift method. If the rescuers open the airway, and hear gurgling sounds, the medics will log roll the patient and suction the oropharynx to clear the airway. The airway must be clear before any further assessment is considered.
Assess breathing
After the patency of the airway has been assured, the patient’s breathing is assessed. If the patient is unresponsive, there is a very possible that the patient needs positive pressure ventilation. If the patient is not alert, assessment of the rate, rhythm, and quality of respiration is made. If a patients respirations are shallow, too fast, or too slow, positive pressure ventilation is indicated. It seems counterintuitive to ventilate a patient who is breathing, but when a patient is only breathing 4 times a minute or barely moving any air because they are breathing 40 times a minute and unresponsive, the patient won’t be moving enough air to stay alive for any reasonable period of time. For this reason the EMS crew is should always be ready to ventilate an unresponsive patient. Sometimes the patient is unconscious and the breathing is normal. In these cases, nothing is required. Similarly, if the patient is alert and demonstrates any respiratory distress or increased work of breathing, oxygen is administered via non rebreather mask. Administering high flow oxygen to patients with demonstrated respiratory distress will buy the ambulance crew a little time to determine the underlying cause of the breathing problem and begin treatment. When patients are having problems breathing, regardless of cause, oxygen is the first and best treatment to initiate.
Assess circulation
Assessing the patient’s radial pulse gives the ambulance crew a clue about the patient’s blood pressure. Shock is a major concern of EMS. Patients in shock often descend into cardiac arrest prior to arrival at the hospital. Early identification and timely treatment of shock will turn the odds of survival in favor of the patient. Further, moving a patient in shock should be undertook as gently as possible to prevent the patient from decompensating while even moving the patient to the ambulance. In the simplest terms, shock is hypoperfusion. If a patient’s blood pressure is too low, cellular respiration will be reduced, leading to cell dysfunction and death. If the patient does not have a radial pulse, they are in shock and treatment should be immediate. Treatment for shock includes high flow oxygen administration, elevation of the feet (when possible), and covering the patient with a blanket to prevent heat loss. Numerous conditions can result in shock, it does not have to be a traumatic injury that results in this condition.
Other clues are available to the ambulance crew. Cyanosis (blue skin), cold skin temperature, and dry skin could mean shock in an adult. A very reliable finding in a pediatric patient is slow capillary refill time. Capillary refill time is calculated by pressing the fingertip with your finger and counting the number of seconds until the fingertip or fingernail color returns to normal. Normal is 2 seconds, anything longer is delayed. Delayed capillary refill time in a pediatric patient most often means shock.
In addition to assessing the radial pulse, assessing for major bleeding (this is different than the apparent life threat, which was spurting blood) and stopping the bleeding is critical at this stage. Stopping bleeding is accomplished with direct pressure. Direct pressure may have to continue throughout the movement of the patient to the ambulance and even the ride to the hospital. For this, the EMS crew may opt to delegate this role to another rescuer.
Choose a follow up assessment
Based on the presence of a MOI from the scene size up, it may make more sense to look for injuries. Looking for injuries is accomplished with the rapid trauma assessment. If there is no MOI, and the patient is conscious then it would make more sense to ask questions. EMS will ask questions and perform further assessment guided by the focused history and physical exam.
