Management of Inadequate Ventilation
Published (updated: ).

When the patient is unresponsive and demonstrates any deficiencies with rate, rhythm, or quality in breathing, the patient probably needs to be ventilated with a pocket face mask or bag valve mask. The easiest and smallest device that would give the provider the ability to ventilate without performing mouth to mouth resuscitation is a pocket face mask.
A pocket mask is a small portable device used in the pre-hospital setting to provide adequate ventilation to a patient whom is either in respiratory failure or cardiac arrest. The pocket mask is designed to be placed over the face of the patient, thus creating a seal enclosing both the mouth and nose. Air is then administered to the patient by an emergency responder. The emergency responder exhales through a one-way filter valve, providing adequate ventilation to the patient. The emergency responder is capable of delivering up to 16% oxygen with his/her breath.
Modern pocket masks have either a built in one-way valve or an attachable, disposable filter to protect the emergency responder from the patient’s potentially infectious bodily substances, such as vomit or blood.
Many masks also have a built-in oxygen intake tube, allowing for administration of 50-60% oxygen. Without being hooked up to an external line, exhaled air from the provider can still provide sufficient oxygen to live, up to 16%. Earth’s atmosphere consists of approximately 21% oxygen.
While a pocket mask is not as efficient as a bag valve mask, it does have its advantages when only one rescuer is available. As suggested by its name, the pocket mask benefits from a somewhat easier portability when compared to the bag valve mask. Also, in contrast to the bag valve mask, which requires two hands to operate (one to form a seal and the other to squeeze the bag), the pocket mask allows for both of the rescuer’s hands to be on the patients head. This hand placement provides a superior seal on the patient’s face, and allows the responder to perform a jaw thrust on patients who may have a spinal injury.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or “self-inflating bag”, is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that “all healthcare providers should be familiar with the use of the bag-mask device.” Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
Use of manual resuscitators to ventilate a patient is frequently called “bagging” the patient and is regularly necessary in medical emergencies when the patient’s breathing is insufficient (respiratory failure) or has ceased completely (respiratory arrest). Use of the manual resuscitator force-feeds air or oxygen into the lungs in order to inflate them under pressure, thus constituting a means to manually provide positive-pressure ventilation. It is used by professional rescuers in preference to mouth-to-mouth ventilation, either directly or through an adjunct such as a pocket mask.
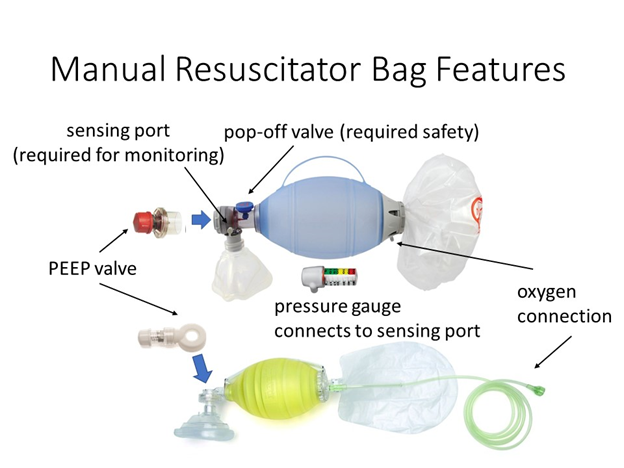
The BVM consists of a flexible air chamber (the “bag”, roughly a foot in length), attached to a face mask via a shutter valve. When the face mask is properly applied and the “bag” is squeezed, the device forces air through into the patient’s lungs; when the bag is released, it self-inflates from its other end, drawing in either ambient air or a low pressure oxygen flow supplied by a regulated cylinder, while also allowing the patient’s lungs to deflate to the ambient environment (not the bag) past the one way valve.
Bag and valve combinations can also be attached to an alternative airway adjunct, instead of to the mask. For example, it can be attached to an endotracheal tube or laryngeal mask airway. Small heat and moisture exchangers, or humidifying/bacterial filters, can be used.
A bag valve mask can be used without being attached to an oxygen tank to provide “room air” (21% oxygen) to the patient. However, manual resuscitator devices also can be connected to a separate bag reservoir, which can be filled with pure oxygen from a compressed oxygen source, thus increasing the amount of oxygen delivered to the patient to nearly 100%.
Bag valve masks come in different sizes to fit infants, children, and adults. The face mask size may be independent of the bag size; for example, a single pediatric-sized bag might be used with different masks for multiple face sizes, or a pediatric mask might be used with an adult bag for patients with small faces.
Manual resuscitators cause the gas inside the inflatable bag portion to be force-fed to the patient via a one-way valve when compressed by the rescuer; the gas is then ideally delivered through a mask and into the patient’s trachea, bronchus and into the lungs. In order to be effective, a bag valve mask must deliver between 500 and 600 milliliters of air to a normal male adult patient’s lungs, but if supplemental oxygen is provided 400 ml may still be adequate. Squeezing the bag once every 5 to 6 seconds for an adult or once every 3 seconds for an infant or child provides an adequate respiratory rate (10–12 respirations per minute in an adult and 20 per minute in a child or infant).
Professional rescuers are taught to ensure that the mask portion of the BVM is properly sealed around the patient’s face (that is, to ensure proper “mask seal”); otherwise, pressure needed to force-inflate the lungs is released to the environment. This is difficult when a single rescuer attempts to maintain a face mask seal with one hand while squeezing the bag with other. Therefore, common protocol uses two rescuers: one rescuer to hold the mask to the patient’s face with both hands and focus entirely on maintaining a leak-proof mask seal, while the other rescuer squeezes the bag and focuses on breath (or tidal volume) and timing.
Under normal breathing, the lungs inflate under a slight vacuum when the chest wall muscles and diaphragm expand; this “pulls” the lungs open, causing air to enter the lungs to inflate under a gentle vacuum. However, when using a manual resuscitator, as with other methods of positive-pressure ventilation, the lungs are force-inflated with pressurized air or oxygen. This inherently leads to risk of various complications, many of which depend on whether the manual resuscitator is being used with a face mask or ET tube. Complications are related to over-inflating or over-pressurizing the patient, which can cause: (1) air to inflate the stomach (called gastric insufflation); (2) lung injury from over-stretching (called volutrauma); or (3) lung injury from over-pressurization (called barotrauma).
When a face mask is used in conjunction with a manual resuscitator, the intent is for the force-delivered air or oxygen to inflate the lungs. However air entering the patient also has access to the stomach via the esophagus, which can inflate if the resuscitator is squeezed too hard (causing air flow that is too rapid for the lungs to absorb alone) or too much (causing excess air to divert to the stomach).” Gastric inflation can lead to vomiting and subsequent aspiration of stomach contents into the lungs, which has been cited as a major hazard of bag-valve-mask ventilation, with one study suggesting this effect is difficult to avoid even for the most skilled and experienced users, stating “When using a self-inflatable bag, even experienced anesthesiologists in our study may have performed ventilation with too short inspiratory times or too large tidal volumes, which resulted in stomach inflation in some cases.

The Sellick Maneuver is performed by applying gentle pressure to the anterior neck (in a posterior direction) at the level of the Cricoid Cartilage. The Maneuver is most often used to help align the airway structures during endotracheal intubation. The real value of this procedure is often misunderstood and therefore, is often underutilized. The REAL value of the Sellick Maneuver is to provide a means to prevent gastric insufflation and vomiting during ventilations in an unprotected airway. BLS and ALS medics can direct a member of the resuscitation team to provide this maneuver early and continually until a properly placed endotracheal tube has been inserted. Remember that aspiration pneumonitis has a high mortality rate and proper use of this method can minimize its occurrence.
Patients who are not alert are the ones that usually need to be ‘bagged’
Patients who are not alert and not talking need to have their airway assessed by opening the airway and looking, listening, and feeling for breathing. Once the airway has been determined to be clear, assess breathing. If the patient is breathing faster than 20 breaths per minute or less than 12 breaths per minute or the rhythm is irregular, this patient requires ventilation. If the patient is not alert, care must be taken to ensure then airway remains clear during transport. Steps that can be taken are:
- Positioning the patient in the left lateral recumbent position
- Using the bag valve mask to simply administer oxygen
- By constantly observing the patient mouth during transport
