Assessment of Adequate and Inadequate Ventilation
Published (updated: ).
The primary survey is where we figure out if the patient is conscious or needs ventilation
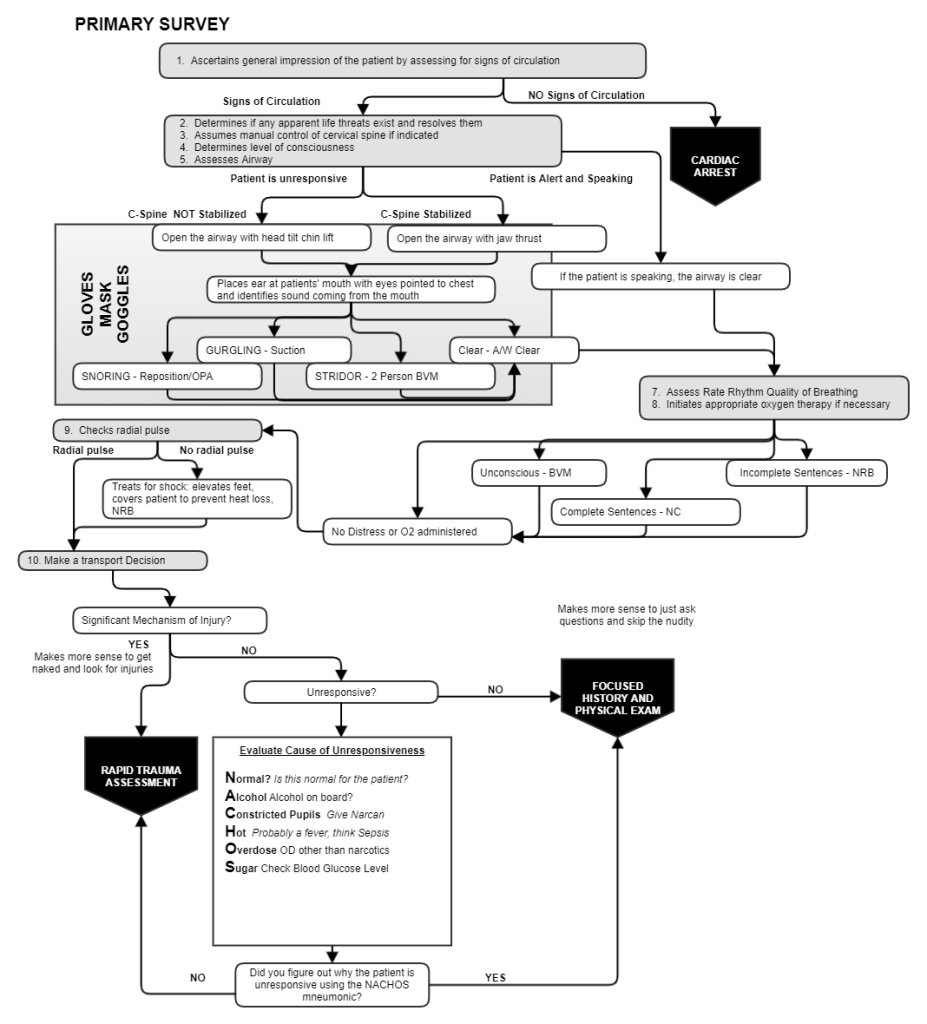
During the primary survey, the ambulance crew meets the patient face to face and makes some quick observations. Is the patient conscious and talking? If so the airway is clear. Is the patient not alert (not talking)? Then the airway requires assessment. Despite the fact that patients who are alert and talking are literally telling the EMS crew that their airway is clear, the patient could still be having difficulty breathing.
Patients who can talk to you probably won’t let you bag them
Patients who are talking could still have difficulty breathing. Does this mean that they need to be ventilated with a bag valve mask? The answer is usually no. What patients who are talking and appear to be experiencing difficulty in breathing need is supplemental oxygen. The idea behind supplemental oxygen is the air the patient breathes contains a higher concentration of oxygen than the environment. Supplemental oxygen is given either by non rebreather mask or nasal canula. By increasing the inspired oxygen levels, the patient’s respiratory distress can be decreased, which will allow time for further examination. Further, administering supplemental oxygen may decrease the chances that the patient will deteriorate before the patient is transported to the hospital.
Assess breathing by determining the rate, rhythm, and quality of breathing
To determine the rate, the medics need to check the respiratory rate. The idea is to determine how many breaths the patient takes every minute. For an adult, the normal respiratory rate would be between 12 and 20 breaths per minute. To arrive at the minute rate in less than a minute, simply count the number of breaths the patient takes in 15 seconds and multiply x 4. For example, if the patient is breathing 4 times in 15 seconds, the minute rate would be 16 breaths per minute. Well within normal limits.
When counting the rhythm, determine if the breaths are happening at consistent intervals. Breathing by it’s very nature is very regular, irregular respiratory patterns are important could point to a much bigger problem, or cause the medics to be concerned that the patient will just stop breathing altogether before making it to the hospital.
Quality is observed by looking at the amount of movement the chest makes when the patient breathes. If the chest is barely moving, the quality would be described as shallow. If the chest appears to move really slowly (indicating the patient is struggling to expand their lungs), the quality would be described as labored. If the patient has normal expansion of the chest with no effort, the respirations would be described as normal.

Other signs of inadequate breathing
When the breathing can be described as labored, further assessment could reveal the following:
- Accessory muscle usage – The respiratory effort is creating a vacuum that pulls the skin closer to the ribcage exposing the accessory muscles of respiration. This observation is called retraction.
- Nasal flaring – when the patient takes a breath, do they flare their nostrils? This unconscious measure taken by the patient opens the nose to take in just a little more air.
- Abdominal breathing – Infants breathe with their abdomen for the same reason adults would breathe with their abdomen – the muscles of the chest aren’t getting the job done.
- Patient found in upright position – The natural position a patient takes when they are having problems breathing is upright. This measure takes any unnecessary weight off the chest to allow the patient to breathe easier. The patient may even be sitting upright but leaning forward. This position is referred to as the tripod position. Patient’s found in the tripod position are demonstrating profound respiratory distress.
- Fatigue – Fatigue is noticed when the patient appears tired. Fatigue causes the patient to move slowly and seem exhausted by moving only the weight of their body.
- Noisy breathing – Breathing is supposed to be quiet. When it’s not, there is a problem. Noises one could encounter could be stridor (high pitched sound from the mouth), or wheezing (high pitched sound from the lungs on exhalation).
- Visible damage to the chest wall – Damage from multiple broken ribs (flail chest) could result in paradoxical respirations (each lung expanding in opposition to the other). When a patient has a broken rib, they will often ‘splint’ the chest wall with their arm. The act of self splinting is natural.
Ventilation is about moving air, oxygenation is about oxygen in blood
Clues abound for medics considering problems with ventilation are the origin of the patient’s shortness of breath. Problems with ventilations are only one cause of a patients difficulty breathing. Oxygenation is another. Oxygenation refers to oxygen in the air actually getting into the blood. Patients breathing air that is either low in oxygen (poison gas or enclosed space) or air pressure (like high altitudes) could cause problems with oxygenation. Problems with the pulmonary capillaries could fail to absorb oxygen from the atmosphere. How could the medics determine the patient is experiencing poor oxygenation?

Normal oxygenation is observed with the patient has normal mental status and normal skin color. Normal mentation is characterized by a patient who is alert and speaking. Less than normal mentation would be characterized as alert to verbal stimuli, painful stimuli, or unresponsive. Less than optimal skin color would be cyanosis (blue), pale, or mottled (mix of cyanosis and normal)
